Studies specifically designed to evaluate prevalence of statin-related myalgia have shown that approximately 22% of patients on statins have some degree of musculoskeletal pain.1 As clinicians, we know it is difficult for patients to discern between pain related to statin intolerance and that associated with aging, osteoarthritis or autoimmune disorders. Many patients with these symptoms discontinue their statin medication without consulting their primary care provider. This likely leads to increased cardiovascular disease (CVD) risk related to medication non-compliance.
Low serum concentrations of 25-hydroxyvitamin D (< 20 ng/ml) are independently associated with myalgia2,3 and there is a possible connection between statin intolerance and vitamin D deficiency. Bioactive vitamin D, or calcitriol (1, 25-(OH) 2D3), is a steroid hormone that has an essential role in bone mineralization. However, recent data shows that vitamin D receptors have been identified in a wide variety of cells, demonstrating that this hormone’s biological involvement may well extend beyond mineral metabolism.4 The function of vitamin D at the cellular and genomic levels may explain the hormone’s possible role in diseases such as multiple sclerosis, depression, tuberculosis, CVD, asthma and cancer.5,6 It is reported that vitamin D deficiency is more prevalent than previously recognized and may be present in 50% of the adult population.7
In my own clinical practice dealing with lipid disorder patients, I began seeing an association between vitamin D deficiency and reported intolerance to statins. Vitamin D levels were measured as part of a retrospective chart review of lipid outcomes in patients seen in my lipid clinic. This allowed me to track my presumption that an association may exist between a deficiency in vitamin D and intolerance to statin medications. This association led to a review of the literature and a closer look of patients already enrolled in a six-month pilot study within my practice.
From this literature review there appears to be different concepts related to the potential mechanisms by which vitamin D and statins may be connected to patient intolerance. Vitamin D insufficiency may potentiate statin-induced myalgia and/ or statins themselves may contribute to vitamin D deficiency. As of this review, there have been several non-blinded studies that support the concept that vitamin D deficiency may be directly
related to statin-induced myalgia. Ahmed et al.8 reported in 2009 the resolution of statin-induced myalgia in 92% of vitamin D-deficient patients after vitamin D supplementation. In a small case series published in 2010 by Dr. David Bell,9 four of six patients with statin-induced myalgia and vitamin D deficiency who were rechallenged with the same statin dosage after the correction of vitamin D levels tolerated the statin for at least six months. In a review, Lee et al.10 also highlighted the association of vitamin D insufficiency with statin-induced myalgia, demonstrating successful re-introduction of statin therapy in a subgroup of patients following appropriate repletion of vitamin D levels. Literature also reports that insufficient cytochrome P450 (CYP) enzyme activity related to vitamin D deficiency may be responsible for inactivity and increased toxicity of CYP-metabolized statins in some patients, leading to the need for possible statin dose adjustments.11
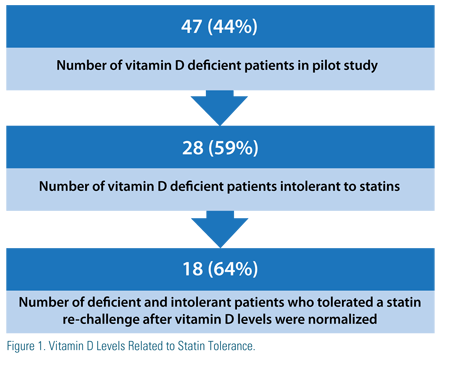 Reviewing the data from my own six-month pilot study (Figure 1), I found that 106 (70%) of 151 lipid patients had vitamin D levels assessed as part of their initial workup. Of these patients, 47 (44%) had vitamin D levels of less than 30 ng/ dl. The number of vitamin D-insufficient patients intolerant to statins was 28 (59%). Most notably, the number of vitamin D-deficient and -intolerant patients who – after achieving normal vitamin D levels with supplementation – were able to tolerate the re-challenge of a statin for at least six months was 18 (64%).
Reviewing the data from my own six-month pilot study (Figure 1), I found that 106 (70%) of 151 lipid patients had vitamin D levels assessed as part of their initial workup. Of these patients, 47 (44%) had vitamin D levels of less than 30 ng/ dl. The number of vitamin D-insufficient patients intolerant to statins was 28 (59%). Most notably, the number of vitamin D-deficient and -intolerant patients who – after achieving normal vitamin D levels with supplementation – were able to tolerate the re-challenge of a statin for at least six months was 18 (64%).
The data are certainly evolving related to vitamin D deficiency and it relationship to CVD risk as a whole. Vitamin D deficiency potentially is associated with hypertension, diabetes and the metabolic syndrome, left ventricular hypertrophy, congestive heart failure and chronic vascular inflammation.12,13 In a recent meta-analysis of 18 randomized controlled trials of 57,000 subjects, a vitamin D intake of > 500 IU/day was associated with lower allcause mortality, in part by association with fewer CV deaths.14
This information, along with the small non-blinded studies and anecdotal observations that repletion of 25 (OH) D levels predictably improves or resolves statin-related myalgia, certainly warrants a further look at how we treat our lipid patients who are already at increased CVD risk. Statins are the cornerstone for the prevention and treatment of coronary heart disease. Strategies to improve tolerance of and compliance with these medications are essential; thus, supporting the suggestion that vitamin D may be is an excellent option for this statin intolerant patients with inadequate Vitamin D, thus, supporting the suggestion that vitamin D may be an excellent option for statin intolerant patients with inadequate vitamin D.
Disclosure statement: Debra Friedrich has received honoraria from Amarin Corporation.






.jpg)
.png)











