According to the 2011 National Diabetes fact sheet, 25.8 million adults and children in the United States (8.3%) have diabetes and 79 million have pre-diabetes. In 2010 alone, 1.9 million new cases of diabetes were diagnosed. In 2007, the total cost of diagnosed diabetes was $174 billion and contributed to more than 231,000 deaths in the U.S.1
Diabetes Means Cardiovascular Disease and More
Diabetes mellitus (DM) leads to twofour times greater risk for stroke and CVD deaths. Two-thirds of them have hypertension (blood pressure >140/90 or taking medications). It is the leading cause of new cases of blindness; 28.5% (4.2 million) had retinopathy.
DM is the leading cause of kidney failure, accounting for 44% of new cases in 2008. Sixty to seventy percent of people with diabetes have some form of neuropathy. Sixty percent of non-traumatic lower limb amputations occur in people with diabetes.1
How can we tackle this problem? We are in the 21st Century with EHR (electronic health records) at our fingertips. What works the best? What evidence do we have? How do we approach it? In a recent Annals of Internal Medicine article, the authors concluded that the use of a commercially available certified EHR was associated with improved drug treatment intensification, monitoring, and significant improvements in A1C and LDL cholesterol. Greater improvements were seen among patients with worse control of HbA1C (> 9%) and LDL (>130).2
A multifactorial approach to diabetes care that includes an emphasis on blood pressure, lipids, glucose, aspirin use and non-use of tobacco will maximize health outcomes far more than a strategy that is limited to just one or two of these clinical domains.1,3-6 The benefits of a multifactorial approach to diabetes care are supported by the results of the Steno 2 Study of 160 patients with type 2 diabetes and microalbuminuria. Multifactorial interventions achieved a 50% reduction in mortality and significant reduction in microvascular complications five years after the end of a 7.8-year study. Multifactorial intervention achieved A1c of 7.8%, LDL of 83 mg/dL, and blood pressure of 131/73, compared to a conventional group that achieved A1c 9%, LDL 126 mg/dL and blood pressure 146/78.5
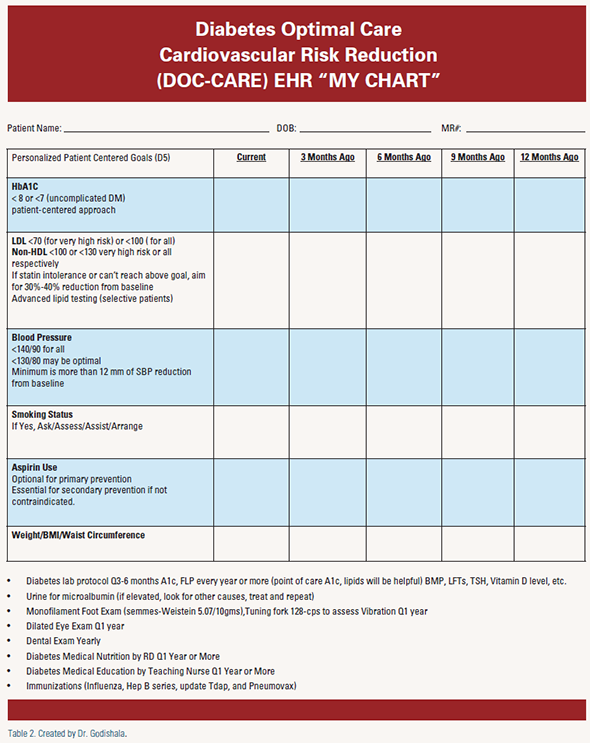
In Minnesota, Community Health Measures report D5 scores of participating clinics (“D5”= A1C <8, LDL <100, blood pressure <140/90, aspirin use, non-use of tobacco). Reaching all five goals (D5) greatly reduces a patient’s risk for the microvascular and cardiovascular problems associated with diabetes.7
Optimal glycemic control, blood pressure, aspirin use and management of diabetic dyslipidemia are still evolving and moving targets.
Glycemic Control
A new position statement in October 2012 from European Association for the Study of Diabetes and American Diabetes Association for the treatment of type 2 diabetes takes an approach much more focused on the individual patient compared with the “one number fits all” target of glycated hemoglobin (HbA1c) used up to now. Diet, exercise and education are the foundation of the treatment program. Metformin is used as the optimal first line drug unless contraindicated. Lowering HbA1C to below or around 7% has been shown to reduce microvascular complications, and if implemented soon after the diagnosis of diabetes, is associated with a long term reduction in macrovascular disease. Therefore, a reasonable HbA1c goal for many nonpregnant adults is <7%. Less stringent A1c goals (such as <8%) may be appropriate for patients with a history of severe hypoglycemia, limited life expectancy, advanced microvascular or macrovascular complications, extensive comorbid conditions, and those with longstanding diabetes in whom the lower goal is difficult to attain despite appropriate glucose monitoring, and effective doses of multiple glucose-lowering agents including insulin.1,3
Diabetic Dyslipidemia
Seventy to seventy-five percent of adult patients with diabetes die of macrovascular disease. They develop more atherosclerosis than patients without diabetes with the same quantitative lipoprotein profiles. For diabetic dyslipidemia, achieving an LDL goal of less than 100 alone is not optimal. More focus and attention towards shifting the atherogenic dyslipidemia of pattern B to pattern A, as well as aggressive reduction of LDL particle number or achieving optimal apoB levels, is ideal but not yet the standard of care, and performing these tests in every patient is not cost effective. A reasonable approach would be achieving both LDL and non-HDL goal for all diabetic patients along with the other four measures of D5. The beneficial effects of statins on cardiovascular risk reduction may go beyond their effects on lipid levels.1,3 TLC (therapeutic lifestyle changes) and effective doses of statins for all patients is a minimum. If patients cannot tolerate trials of multiple statins to achieve at least a 30-40% reduction of both LDL and non-HDL from baseline, one should individualize the choice of non-statin medications based on patients’ comorbidities and DDIs (drug-drug interactions). High triglycerides and low HDL cholesterol levels are independent risk factors for cardiovascular disease in the patient with diabetes. Individuals with elevated triglycerides may achieve significant cardiovascular risk reduction with the use of fibrates8 or statins.9 Current evidence does not support the use of combination therapy with statins and other lipid-lowering drugs for most patients with type 2 diabetes. The combination of a statin plus ezetimibe versus statin monotherapy has not yet been shown to be advantageous.10
The ACCORD study showed no significant reduction in myocardial infarction, stroke or cardiovascular death with a fibratestatin combination compared to statin monotherapy. However, a subgroup analysis suggested a possible benefit for men and women with both low HDL (< 34 mg/dL) and elevated triglycerides (> 204 mg/dL). In AIM-HIGH, niacin/ statin combination therapy did not show benefit and was stopped early due to futility. Upcoming ATP IV guidelines, pending major clinical trials data, and new classes of drugs/novel therapies may influence future management of diabetic dyslipidemia.
Blood Pressure Control
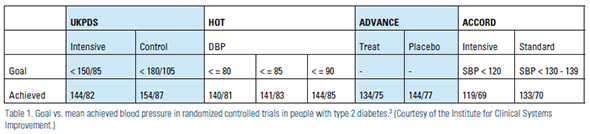
In type 1 diabetes, hypertension is often the result of underlying nephropathy, while in type 2 diabetes it usually coexists with other cardiometabolic risk factors. There is no definitive evidence for any particular general blood pressure goal for patients with diabetes. Epidemiologic analyses have shown that blood pressures >115/75 mmHg are associated with increased cardiovascular event rates and mortality in individuals with diabetes.13,14 RCT's have demonstrated the benefit (reduction of CHD events, stroke, and nephropathy) of lowering blood pressure to <140/80mmHg in individuals with diabetes.13,15-17 The UKPDS, HOT, and ADVANCE trials compared more stringent versus less stringent blood pressure goals and showed reduced major cardiovascular events. However, none of these trials achieved average SBP below 130 mmHg (Table 1). The ACCORD trial found no difference in major cardiovascular outcomes between a more intensive blood pressure < 120 mmHg (achieved 119/69) compared to standard intervention targeting systolic blood pressure between 130 and 139 mmHg (achieved 133/70).
Intensive blood pressure regimens were associated with a small reduction in the rate of stroke, greater medication use (3.4 vs 2.1) and more serious adverse events. A post hoc analysis of the INVEST (International Verapamil/Trandolapril) Study of blood pressure control (6,400 patients with diabetes and CAD) demonstrated that “tight control” (<130 mmHg) was not associated with improved cardiovascular outcomes compared with “usual care” (130–140 mmHg).18
SBP targets <130 or <140 mmHg may be appropriate for individual patients, based on response to therapy, medication tolerance, and individual characteristics. Based on pooled data from RCT's, an average reduction of SBP by 12-13 mm of Hg over four years was associated with 21% reduction in CHD, a 37% reduction in stroke, a 25% reduction in total cardiovascular mortality and a 13% reduction in all-cause mortality.19 Urinary albumin excretion should be tested annually and treated if abnormal. RAAS (ACE or ARB) blockers with or without diuretics or calcium channel blockers are appropriate first line agents if not contraindicated. JNC VII and ADA recommended a blood pressure goal of less than 130/80 in diabetics. Upcoming JNC VIII guidelines and future ADA& NKF guidelines may shed more light on targeting blood pressure goals for diabetic patients. For now, the goal for all diabetic patients is less than 140/90, with an optional goal of less than 130/80, with a minimum 12 mm of SBP reduction from baseline.
Aspirin Use
There is insufficient evidence to recommend for or against aspirin use in the primary prevention of cardiovascular events in patients with type 2 diabetes. There is sufficient evidence to support the use of aspirin for secondary prevention (i.e., EDTRS, HOT, Harpaz, et. al, and other systematic and narrative reviews by Sirois, et. al).1,3 In Steno-2 it was difficult to assess if aspirin use was beneficial. However, aspirin is no longer recommended for those at low CVD risk (women under age 60 years and men under age 50 years with no major CVD risk factors or a 10-year CVD risk <5%), as the benefit is likely to be outweighed by the risk of significant bleeding. Clinical judgment should be used for those at intermediate risk (10-year CVD risk of 5–10%) until further research is available.1,3 Recent trials of aspirin use in diabetes have shown less benefit than older trials (perhaps due to better background A1c, blood pressure, and LDL control and lower smoking rates in recent trials).3,11 There are significant limitations identified in all of these studies, and more definitive studies would be helpful.12 Therefore, based on current evidence, low-dose aspirin is considered optional for primary prevention.
Smoking Cessation
Tobacco cessation is very likely to be the single most beneficial intervention that is available. Ask, Advise, Assess and Arrange follow-up referral to special programs or pharmacotherapy. A meta-analysis of 20 prospective cohort studies demonstrated a 36% relative risk reduction in mortality for coronary heart disease patients among individuals who quit smoking as compared to those who continued to smoke.20 Much of the documented impact of smoking on health does not separately address patients with diabetes, but suggests that the benefits are at least equivalent to those found in the general population. Tobacco telephone quit lines: HHS National Quit line (1-800-QUITNOW) or 1-800-784-8669 connect to counseling and information about quitting smoking in your state.
Diabetes is a complex, chronic disease which requires a lifelong partnership between the health care team and patient. Until we track and implement various goals we will not stop the progression of this deadly disease (Table 2). Most commercial EHRs like EPIC have easy tracking capabilities. This requires teamwork, leadership and resources. Smart patient registries can help to identify, monitor and prioritize goals. In addition to office visits, follow-up phone calls, send “my chart” messages, e-mails and utilization of modern texting may all be required. As we have seen with the success of Get with the Guidelines by AHA's CAD program, creating a personalized, web-based MY DIABETES CARE on MY CHART and having it POP UP each visit and every time the patient opens his or her “my chart” can be tremendously effective. In this day and age, more and more patients are accessing “my chart” to view their health history, medications, immunizations and lab results. Creating a personalized “my diabetes” page with an automatic or manually updated tracking system can motivate our patients and improve outcomes.
Disclosure statement: Dr. Godishala has no disclosures to report.
References for this article are listed on Page 31 of Lipid Spin PDF available here.






.jpg)
.png)











