Discuss this article at www.lipid.org/lipidspin
Diabetes mellitus (DM) is a leading cause of cardiovascular disease (CVD) and its associated morbidity and mortality.(1) DM confers the highest lifetime risk of any individual risk factor for developing cardiovascular disease. Although morbidity related to microvascular complications such as retinopathy, nephropathy and neuropathy is common, diabetic individuals are at the highest risk for macrovascular complications.(1) Patients with type 2 DM have a twofold to fourfold increase in risk of incident coronary heart disease and ischemic stroke and a 1.5-fold to 3.6-fold increase in mortality.(2) Some 80% of individuals with type 2 DM ultimately will succumb to death from a cardiovascular cause compared to 30% of the non-diabetic population.(3) This association is further compounded by the fact that multiple metabolic risk factors for atherosclerotic CVD (ASCVD) commonly are found in patients with diabetes.(4)
As such, prevention of ASCVD through comprehensive management of risk factors is critically important, because control of risk factors through intensive medical therapy has been shown to have a strong inverse relationship with risk of death, myocardial infarction and stroke in this population.(5) Additionally, given the occurrence of a first ASCVD event in diabetics is associated with increased morbidity and mortality as compared to the general population, even higher emphasis should be placed on primary prevention in this population. Unfortunately, comprehensive CVD risk factor control remains suboptimal in a majority of diabetic individuals. A study by Wong, et al., showed that, despite approximately 50% of diabetic patients being at goal for either hemoglobin A1c (HbA1c), blood pressure or low-density lipoprotein cholesterol (LDL-C), only 24% of these patients were at goal for all three risk factors.(6) This article will highlight the importance of cardiovascular risk reduction in diabetics, with a particular emphasis on treatment recommendations from the 2018 Multisociety Cholesterol Guidelines.
Health Behaviors
Lifestyle therapies are the cornerstone of ASCVD risk reduction in diabetics and are emphasized in the 2018 guidelines. Smoking cessation and weight reduction are imperative. Individuals should be following a dietary pattern
that emphasizes vegetables, fruits, whole grains, legumes, healthy protein sources and vegetable oils. Food that should be limited includes processed sugar, sugar-sweetened beverages and red meats. Regular aerobic physical activity five times a week, lasting on average 40 minutes per session and involving moderate to vigorous intensity is recommended, in addition to reducing sedentary behavior.
Lifestyle modification is important in both people with diabetes and those at risk of diabetes. Statins can contribute to the risk of overt DM in people with predisposing risk factors (metabolic syndrome, impaired fasting glucose, obesity or HbA1C greater than 6%), but this should not be a contraindication to treatment in those at increased risk. This is an opportunity to intensify diabetes prevention efforts in these individuals.(8)
Pharmacologic lipid management
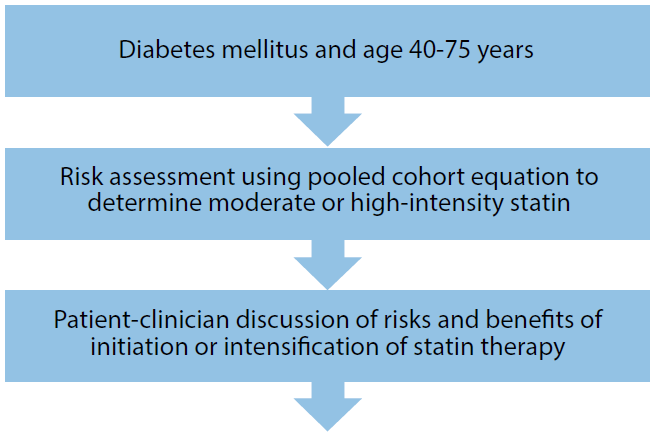
The consistent risk reduction with statins in diabetics is well-established.(8-12) In a meta-analysis of the Atherosclerosis Risk in Communities (ARIC) study, the MultiEthnic Study of Atherosclerosis (MESA) and Jackson Heart Study (JHS) to examine CHD and CVD events in patients with DM, individuals treated with statins had a 41% and 33% risk reduction in coronary heart disease and CVD events, respectively.(13) As such, the 2018 cholesterol guidelines have provided updated guidance regarding goals for lipid management in this highrisk population that is similar to the 2013 AHA/ACC Cholesterol Guidelines.(14) For secondary prevention, the maximally tolerated statin dose is recommended, ideally with a high-intensity statin with the aim of achieving a 50% or greater reduction in LDL-C levels (Strength of Recommendation I: Level of Evidence A). For primary prevention, all adults ages 40 to 75 with diabetes, regardless of estimated 10-year ASCVD risk, at least a moderate -intensity statin is indicated (Strength of Recommendation: I, level of evidence: A). The suggested clinical decision pathway is included in Figure 1.
Regarding recommendations for statin intensity (i.e. moderate vs. high-intensity), the 2018 guidelines do make slightly different recommendations from the 2013 guidelines. In both guidelines, using the pooled cohort equation (PCE) to aid clinical decision-making in primary prevention risk assessment is emphasized. Prior guidelines recommended high-intensity statins if the 10-year ASCVD risk is ≥7.5%. In contrast, the 2018 guidelines recommend highintensity statin if the 10-year risk is 20% or higher (high risk by the PCE). If there is an intermediate 10-year risk of ASCVD (7.5% to <20%), the presence of multiple risk-enhancing factors or an age of 50 to 75 years can favor the use of high-intensity statins in this population (Strength of Recommendation: IIa; Level of Evidence B-NR).(15,16) Treatment with highintensity statins should focus on an LDL-C reduction of greater than 50%.
An important addition to the 2018 guidelines is the recommendation for use of non-statin therapies if a 50% LDL-C reduction is not achieved with a high-intensity statin (Strength of Recommendation: IIb; Level of Evidence: C-LD). Ezetimibe is the preferred initial agent, given the reduction in cardiovascular events seen in the IMProved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT) and Study of Heart and Renal Protection (SHARP).(17,18) The addition of ezetimibe 10 mg/dL to moderate-intensity statin therapy can achieve the same percent LDL-C lowering as that achieved with high-intensity statin therapy.(17) Since the 2013 guidelines, proprotein convertase subtilisin-kexin type 9 (PCSK9) inhibitors also have shown benefit in lipid-lowering and cardiovascular outcomes in the Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) and Evaluation of Cardiovascular Outcomes After an Acute Coronary Syndrome During Treatment with Alirocumab (ODYSSEY OUTCOMES) trials.(19,20) PCSK9-inhibitors are suggested in the guidelines for high-risk individuals who have not achieved 50% LDL-C reduction with maximally tolerated statin and ezetimibe. Because of the high cost of these medications, a value statement was added to the guideline, underscoring the need for clinicians and patients to factor in cost of drugs relative to risk reduction in determining treatment. Based on 2018 price points, PCSK9-inhibitors were considered a low-value intervention, though this is expected to change inow that the cost of these medications has decreased. Bile acid sequestrants (expected LDL-C lowering of 15% to 30%) also can be considered if the patient has experienced significant side effects with the above therapies or if additional therapy is warranted.
Consideration of statin therapy in diabetics older than 75 and younger than 40 emphasize the importance of individualized therapy. In individuals over 75, a clinicianpatient discussion of risk and benefit of these medications is recommended prior to initiation, given that the benefit may be offset by the limited lifespan and increased susceptibility to adverse events in this age group (Strength of Recommendation: IIb; Level of Evidence: C-LD).(16,21,22) If an individual already is on a statin, it is reasonable to continue the medication after the age of 75, given the results of a meta-analysis of the Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) and Heart Outcomes Prevention Evaluation HOPE-3) trials, which showed benefit in ASCVD reduction in those over 70 years of age (Strength of Recommendation: IIa; Level of Evidence B-NR).(23) In adults ages 20 to 39 with a long duration of diabetes (10 years of type 2 DM or 20 years of type I DM), or in those who have some manifestation of end-organ complications of diabetes (i.e., albuminuria with or without nephropathy, retinopathy, neuropathy or peripheral vascular disease), a discussion regarding initiation of a moderate-intensity statin is reasonable, despite limited data in this age group (Strength of Recommendation: IIb; Level of Evidence: C-LD).(21,22,24-31) An important addition to the guidelines is the recommendation that patient risk should be followed and re-evaluated over time because comorbidities and age (and subsequently risk) increase over a lifetime. (24,27,28) The PCE score does not by itself determine whether a statin should be utilized, but is an important tool in the evaluation of a patient’s global risk and aids a clinician’s judgment regarding the benefit of intensifying a statin. Lifetime risk also should be assessed for those younger than 50 years of age. Importantly, the patient’s values, goals and attitudes regarding medications is emphasized in the new guidelines and should be considered so inclusion of patient preference plays a major role in shared decision-making. Hypertriglyceridemia also is a risk factor associated with patients with DM and metabolic syndrome. In patients older than 20 with moderate hypertriglyceridemia (175 to 499 mg/dL), treating lifestyle factors and the underlying secondary factors (e.g. diabetes) is emphasized (Strength of Recommendation: I; Level of Evidence: B-NR). In adults 40 to 75 years of age with moderate (175 to 499 mg/dL) or severe hypertriglyceridemia (≥500 mg/ dL) and elevated ASCVD risk, a persistently elevated triglyceride level despite lifestyle modification is a factor favoring initiation or intensification of statin therapy (Strength of Recommendation: IIa; Level of Evidence: B-R). An additional lipidmodifying consideration in this population is the prescription of icosapent ethyl. The Reduction of Cardiovascular Events with EPA – Intervention Trial (REDUCE-IT) enrolled 8,179 patients with elevated triglycerides (135-500 mg/dL), of which 29% had DM. The trial demonstrated a 30% reduction in total ischemic events in the group receiving icosapent ethyl.(32) Of note, the median baseline LDL-C of patients in this study was 75 mg/dL and patients already were on stable background statin therapy. Although these results were not available to be included in the 2018 Cholesterol Guidelines, icosapent ethyl should be considered in residual risk reduction, particularly in diabetics with elevated triglycerides.
Comprehensive Diabetes Care
Management of diabetes is complex and requires input from a full team of clinicians – certified diabetes educator, nursing support, endocrinologist, nephrologist, primary care, cardiologist, vascular surgeon, nutritionist, psychologist, podiatrist, ophthalmologist and others – regarding the most appropriate treatment plan for an individual patient. The 2018 guidelines provide a framework to aid clinicians in tailoring therapy to each patient based on comorbidities, patient preferences and even cost to emphasize a true shared decision-making model. The intersection of diabetes care and cardiovascular risk reduction is rapidly emerging given the data regarding sodium glucose transporter-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists that have shown consistent reductions in cardiovascular disease and mortality. In addition to the cornerstones of risk reduction included in this article, appropriate implementation of these novel anti-hyperglycemics will be an important consideration in patients going forward, and we expect commentary and recommendations to be included in the next iteration of national cholesterol guidelines. The identification of patients who will derive the most benefit from these medications has been highlighted in a recent ACC Expert Consensus Decision Pathway.(33) Use of registries, including the National Cardiovascular Data Registry’s PINNACLE and Diabetes Collaborative registries, are important opportunities going forward for improving guidelinedirected therapy and patient safety, as well as future research into improving outcomes in this population.
Disclosure Statement: Dr. Dhindsa has no financial disclosures to report. Dr. Mehta has no financial disclosures to report. Dr. Sperling has no financial disclosures to report.
Official Publication of the National Lipid Association






.jpg)
.png)