Discuss this article at www.lipid.org/lipidspan
Cardiovascular risk stratification is imperfect. There are multiple formulas with receiver operator curve (ROC) values, a measure of discrimination between predicted events and nonevents varying from 0.7 to 0.8. There are multiple risk scores. The Systematic Coronary Risk Evaluation (SCORE) model used in Europe is based on sex, age, systolic blood pressure, total cholesterol and smoking status. The U.S.-based Pooled Cohort Equation incorporates age, sex, race, systolic and diastolic blood pressures, total cholesterol and high-density lipoprotein (HDL) cholesterol, diabetes, smoking status, treatment of hypertension and additional calculation of risk if taking a statin and/or aspirin. The Reynolds Risk Score adds a family history of heart attack before the age of 60, C-reactive protein and hemoglobin A1c (HbA1c) in diabetics. The QRISK2 model, developed in England, includes family history of premature coronary heart disease events, chronic kidney disease (stage 4 or 5), atrial fibrillation, presence of rheumatoid arthritis, postal code as a marker of socioeconomic status, age, sex, ethnicity, smoking status, body mass index (BMI), total cholesterol/HDL ratio, diabetes, systolic blood pressure and a family history.
Development of coronary artery disease is dependent on genetic susceptibility, environmental factors and lifestyle. Genetics account for approximately 60% of inheritability. At present, we evaluate clinical risk factors proximal to overt disease. Family history is a look into all three components of the development of atherosclerosis, although family history on a population level may not significantly improve the C-statistics of a risk equation. In an individual, family history may help identify an as-yet-unknown genetic polymorphism and help incorporate not only genetics but environment and lifestyle.(1)
The following patients are examples of how family history was crucial in their management.
CC is an 18-year-old white male whose father and uncle died suddenly. Both his paternal grandfather and grandmother have premature coronary artery disease (CAD).
His electrocardiogram (EKG) and physical exam were normal with a body mass index (BMI) of 22 . His initial lipids were total cholesterol 130 mg/dL, triglycerides 62 mg/dL, high-density lipoprotein cholesterol (HDL-C) 32 mg/dL, low-density lipoprotein cholesterol (LDL-C) 96 mg/dL and nonHDL-C 98 mg/dL. There were no identified secondary causes of dyslipidemia.
His grandmother was evaluated at age 58. She had cholesterol 198 mg/dL, triglycerides 101 mg/dL, HDL-C 45 mg/dL, LDL-C 133 mg/dL and non-HDL-C 153 mg/ dL. Her 10-year cardiovascular risk using PCE is estimated to be 2.7% and lifetime risk 27%. She had a strong family history of CAD, which was a feature not incorporated into the risk calculation. She was not started on a statin. Her first coronary event was at age 61.
From an epidemiologic perspective, there is an observed inverse relationship between HDL-C and cardiovascular risk. However, mendelian randomization studies have not confirmed the independent role of HDL-C when corrected for LDL-C and triglycerides.(1)
CC’s family history suggests a higher-thanexpected risk for premature CAD and prompted the treatment recommendation for early statin initiation and lifestyle modification. Neither the PCE, the Reynolds Risk Score or the QRISK2 adequately characterize his true risk in this context. A follow-up lipid profile revealed an LDL pattern A and his Lp(a) was 64mg/dl (<30mg/dl), characteristics not addressed in standard risk calculators.
LS is another patient whose condition challenges the presently accepted risk calculators. She is 35, white and a former smoker who presented for risk evaluation. Her father had a myocardial infarction (MI) when he was 49 and had moderately elevated triglycerides and low HDL-C.
LS stopped smoking when she was 31. Her cholesterol was 176 mg/dL, triglycerides were 133 mg/dL, HDL-C was 77 mg/dL and LDL-C was 72 mg/dL. The PCE is not validated for risk calculation under age 40. Other than family history, she had no red flags for increased risk and she was counseled on lifestyle interventions. She enjoyed good health until age 56, when she developed atypical chest pain that prompted further evaluation. Her symptoms were not felt to be cardiac in origin, but she was found to have a coronary artery calcium (CAC) score of 297 Agatston units, placing her in the 90th percentile for her age. An advanced lipid profile revealed a total cholesterol of 136 mg/dL, triglycerides 84 mg/dL, HDL-C 59 mg/dL and LDL-C 73 mg/dL. Her apolipoprotein B (apoB) was 35 mg/dL, lowdensity lipoprotein particles (LDLp) 740 nmol/L, Lp(a) <50 mg/dL and lipoproteinassociated phospholipase A2 (Lp PLA2) 42 nmol/ml/min ( normal <123) Her older sister was found to have the same clinical scenario.
LS does not have an identifiable lipid abnormality, nor does she have any ongoing cardiovascular risk factors except for aging and her family history. She did have a brief period of her life when she was a smoker, during which time significant atherosclerosis formation may have been accelerated. However, her family history is particularly strong for early CAD and identification of genetic markers may be clinically helpful in this scenario.
Evaluating genetic predisposition allows risk stratification before the appearance of traditional risk factors. Genetic predisposition can be modified by appropriate lifestyle modification and treatment of established risk factors. Prevention hopefully can be initiated earlier in people with a known genetic predisposition.
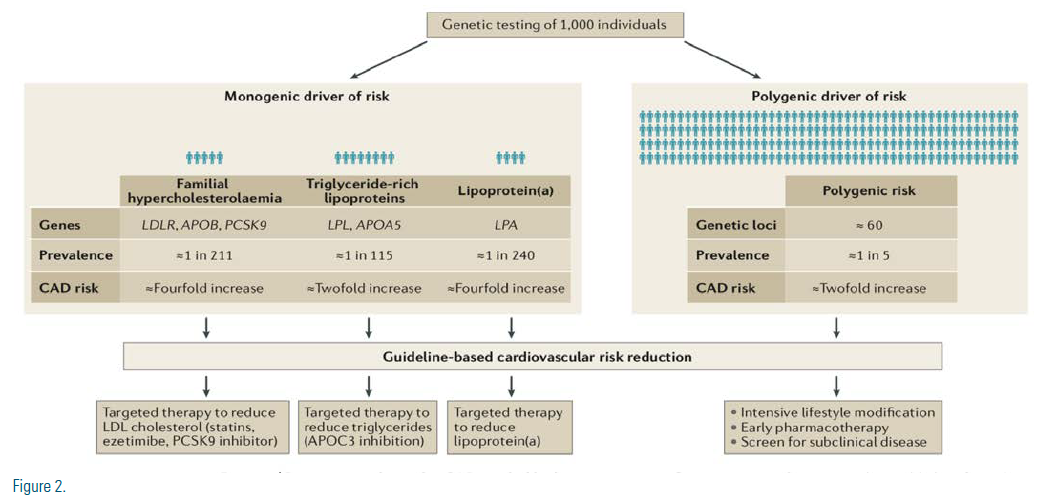
Rare (<0.5 % prevalence) defects in genes that code for important proteins in lipoprotein metabolism account for 1%-2% of premature CAD. Despite the tendency to cluster in families, CAD is a complex and common disorder associated with multiple overlapping genetic variants and should be considered polygenic rather than monogenic in the great majority of cases of premature CAD. To date, there are 164 known single nucleotide polymorphisms (SNPs) associated with the development of cardiovascular disease (CVD).(2) Only half are associated with traditional risk factors. Many are not associated with known pathways of protein production affecting the development of atherosclerosis.(1) (Figure 1)
There are polygenic risk (PGR) scores with a predicted hazard ratio (HR) of 1.5-8.0 similar to monogenic risk determinants.# (Figure 2) Perhaps PGR knowledge for LS and CC would have driven earlier intervention.
TAKE-HOME MESSAGE
ASCVD is a complex, polygenic disease process in which no single risk factor or risk calculator is sufficient in risk stratification. Consideration of family history and potential application of the PGR score into risk assessment may prompt earlier intervention in certain patients, which may lead to better cardiovascular outcomes.
Disclosure statement: Dr. Goldenberg received honoraria from Amarin, Regeneron, and Amgen. Dr. Meng has no financial disclosures to report. Dr. Milea has no financial disclosures to report. Dr. Chawla has no financial disclosures to report.
Official Publication of the National Lipid Association






.jpg)
.png)