Nutrition Recommendations for Hypertriglyceridemia
High triglycerides (TG) are a target for atherosclerotic cardiovascular disease (ASCVD) risk reduction.1-5 Despite the use of statin therapy, ASCVD event rates remain high in patients with elevated TG.1-5 Elevated TG may play a causal role in ASCVD due to an elevation of remnant cholesterol particles.1-5 Elevated TG are associated with an increase in remnant cholesterol, a decrease in high-density lipoprotein cholesterol (HDL-C), and an increase in LDL particles accompanied by an increase in small, dense particles.1-5 The 2018 AHA/ACC/multisociety cholesterol guideline recommended the use of elevated TG as a “risk-enhancing factor” in primary ASCVD prevention.4 The guideline recommended optimizing diet and lifestyle as the first step, ruling out secondary causes of hypertriglyceridemia, and considering statin therapy in those with moderate hypertriglyceridemia and elevated 10-year ASCVD risk. For patients with severe TG elevation (TG > 500 mg/dL and especially those with TG levels > 1,000 mg/dL), primary lowering of TG was recommended to reduce the risk of pancreatitis associated with elevated triglycerides.4
Fasting Versus Non-fasting TG Measurement:
In most patients, the postprandial rise in TG is small, between 12 and 27 mg/dL.1,4 For those with non-fasting TG > 400 mg/dL, a repeat fasting lipid profile is recommended to assess fasting TG and baseline LDL-C. Fasting lipid testing is favored under the following circumstances to establish the diagnosis of the metabolic syndrome, as one of the diagnostic criteria is fasting TG > 150 mg/dL and to identify those with TG > 500 mg/dL as these individuals are at risk for hypertriglyceridemia-induced pancreatitis. Either non-fasting or fasting can be used, though non-fasting levels best capture the average levels over a 24-hour cycle.1,4
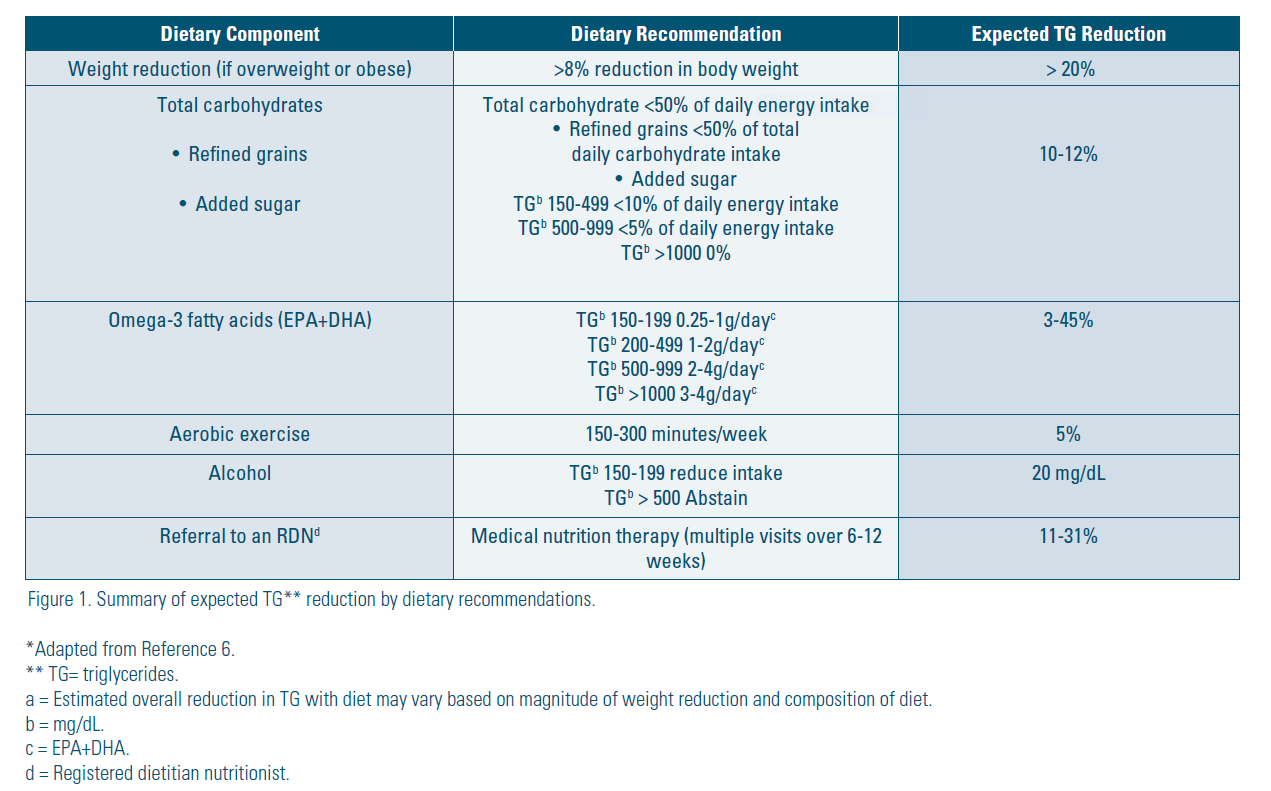
Lifestyle intervention and control of secondary causes are the foundations of TG management.1-8 Dietary intervention can reduce TG levels by 20-50%.1-6 A registered dietitian nutritionist (RDN) can tailor the patients’ dietary recommendations for hypertriglyceridemia.1-11 A summary of expected TG reduction with diet is listed in Figure 1.
Mild to moderate TG elevation is fasting ≥ 150 mg/dL or non-fasting ≥ 175 mg/dL to < 500 mg/dL severe is ≥ 500 mg/dL and especially ≥ 1000 mg/dL.1-6 The higher the TG, the higher the risk of acute pancreatitis.4 In individuals with severe hypertriglyceridemia, a very low-fat diet is required along with a high dose of omega-3 fatty acids and other pharmacotherapy to prevent acute pancreatitis.1-6
Dietary intervention (including weight reduction) and aerobic physical activity are the first line of treatment for hypertriglyceridemia and may be all that is needed for mild to moderate hypertriglyceridemia.1-3,5-8,11 Significant reductions in TG are also achieved with reductions in refined carbohydrate intake together with isocaloric replacement with monounsaturated fat, polyunsaturated fat, and protein1-3,5-8,11, and reducing alcohol in patients with mild to moderately high TG and eliminating it when TG is markedly elevated.1-3,5-8,11 For severe hypertriglyceridemia, the first line of treatment are a very low diet (10-15% of energy intake), physical activity, weight reduction, and pharmacologic treatment.1 Total fat is limited to 20-30 g/day.1-3,5-8,11 which differs from moderate hypertriglyceridemia (30-35% fat and low in saturated fat). For all patients with hypertriglyceridemia, foods with a high-glycemic index (sugar and refined grains) should be limited.1-3,5-8,11
Specific Diet and Lifestyle Recommendations for Lowering TG:
1. Reduce weight if overweight. Weight reduction of 5-10% in individuals with overweight and obesity is a cornerstone of treatment.1-8,11-13 Weight loss of > 8% of total body weight can reduce TG by > 20%.1-8,11-13
2. Increase aerobic exercise. 150-300 minutes of moderate aerobic physical activity per week.1-8,11-13 Aerobic exercise can lower TG by 5%.1-8,11,12
3. Reduce alcohol intake. TG levels increase by 0.2 mg/dL per gram of alcohol consumed daily.14 Reduce consumption if TG are 150-500 mg/dL or elimate if TG > 500 mg/dL.1-8
4. Decrease intake of refined grains and sugar.1-3,5-8,11-13,16 Reducing refined grains (white bread, pasta, white rice) and sugar can decrease TG by 10-25%.1-3,5-8,16 Refined grains should be replaced with whole grains to promote a high fiber intake.1-3,5-8,16
5. Reduce sugar intake. Total carbohydrate (whole grains, fruits and vegetables) intake can be up to 50% of energy intake but sugar intake should be reduced1-3,5-8,16:
• < 10% of energy intake for TG 150-499 mg/dL
• < 5% of energy intake for TG 500-999 mg/dL
• Nearly 0% of energy intake for TG>1000 mg/dL
6. Increase consumption of omega-3 fatty acids. Eicosapentenoic acid (EPA) and docosahexaenoic acid (DHA) can lower TG by 3-45% depending on baseline TG levels and amount of EPA and DHA.1-3,5-8
• TG 150-199 mg/dL: 0.25-1 g/day
• TG 200-499 mg/dL: 1-2 g/day
• TG 500-999 mg/dL: 2-4 g/day
• TG > 1000 mg/dL: 3-4 g/day
The current recommendations for EPA and DHA for the general population is 250 mg/day, equivalent to consuming 8 oz of fatty fish per week.1-3,5-8 Good sources of marine derived omega-3 fatty acids include oily fish such as salmon, mackerel, albacore tuna, trout and sardines.1,2,5-8 Fish oil is an excellent source of EPA and DHA although a prescription dose may be needed for patients who need higher doses.1,2,5-8 An omega-3 supplement that provides 2 to 4 mg/day (EPA + DHA) confers additional TG reduction.1-3,5-8,11 Non-prescription fish oil products are not interchangeable with prescription omega-3 products as they are not approved by the U.S. Food & Drug Administration (FDA) to treat elevated TG levels.1 The content and quality of the supplements can vary and may contain impurities, including saturated fat and oxidized lipids, contaminants, or other harmful ingredients.
7. Referral to an RDN. A systematic review and meta-analysis by Sikand et al. reported that in a pooled analysis of 10 studies, the group counseled by an RDN compared to a control/usual care group had a TG decrease of 15.9 mg/dL, RR: 95%, CI -30.8, -1.1, P=0.014.10 An RDN has the expertise to counsel patients on a very low-fat diet1-3,5-8,18 and to tailor the patients’ diet.
.jpg)
In conclusion, weight reduction (for patients with overweight or obesity), and reducing alcohol, refined grains, and sugar significantly reduces TG. Omega-3 fatty acids and aerobic exercise decrease TG. Personalized nutrition counseling by an RDN will enhance TG reduction. Patients with TG consistently above 1000 mg/dL should be evaluated by a lipidologist to determine the dyslipidemia type and identify the small subset that has Type I. Lifestyle interventions, with many options, are an important tool that can be used to effectively manage patients with hypertriglyceridemia.
Resources
Lifestyle Changes to Reduce Triglycerides
When Your Triglycerides Are over 1000mg/dL
Disclosure statement: Ms. Sikand has no financial disclosures to report. Dr. Kris-Etherton has received honoraria from Humann, Heali, Seafood Nutrition Advisory, McCormick Science Institute, Hass Avocado Board, American Pecan Council, American Pistachio Growers, California Walnut Commission, and Ekaterra Tea.
References are listed on the 2022 Spring LipidSpin .pdf on www.lipid.org






.jpg)
.png)