The NLA now includes > 2,000 members with representation from physicians, NP/PAs, clinical pharmacists, dietitians, and other healthcare professionals. In this Clinical Feature, we highlight the many ways in which our SWLA/PLA members are pushing boundaries in Clinical Lipidology. Across the NLA, professionals of diverse backgrounds share many goals and are all working together to advance this important field:
- We provide expert care in lipidology and CVD prevention.
- Our specialty knowledge and training enables us to push boundaries in medicine, nursing, pharmacology, and nutrition through earlier detection and treatment of lipid disorders and CVD risk factors with a goal of helping to keep people healthy and avoid cardiovascular events and other lipid-related diseases, such as acute pancreatitis.
- We are working toward and advocating for a paradigm shift, where early detection and treatment of cardiovascular risk factors, including lipids, improves the lives of individuals and reduces the burden of CVD in the United States and beyond.
What follows are insights from four healthcare professionals, describing their unique experiences in diverse practice settings, and highlighting the ways in which these lipid specialists are pushing boundaries in Clinical Lipidology:
- Academic setting: Dr. Michael Wilkinson, physician, Director of the University of California San Diego (UCSD) Advanced Lipid Disorders Clinic, describes practice within an academic setting in La Jolla, California.
- Veterans Affairs: Dr. Elizabeth Urteaga, clinical pharmacist, describes practicing Clinical Lipidology as a part of primary care within the Veterans Affairs Health System in San Antonio, Texas.
- Private practice: Ms. Elizabeth Jackson, clinical nurse specialist, Lipid Specialist, describes her experience in private practice in Austin, Texas.
- Pediatrics: Ms. Lauren Williams, registered dietitian, describes practicing in pediatric lipidology at Cook Children’s Medical Center in Fort Worth, Texas.
Dr. Wilkinson, Physician, Academic Lipid Clinic
The Advanced Lipid Disorders Clinic at UC San Diego (UCSD Lipid Clinic) represents one model for a lipid clinic (or preventive cardiology clinic) in an academic medical center. Lipid clinics in academic medical centers are diverse in their structure and focus, with varying levels of clinical and research activity. Lipidology at UCSD has grown out of a combined clinical/research program (Lipid Research Clinic) founded by Drs. Joe Witztum and Dan Steinberg in the 1970-1980’s. Because of work by Dr. Sotirios Tsimikas, Dr. Witztum, and others, UCSD has been at the forefront of basic and translational research in lipidology, especially lipoprotein(a) and oxidized phospholipids. Advances in research led to the development of clinical expertise in the management of patients with elevated lipoprotein(a).1 This is one of the unique aspects of UCSD’s Lipid Clinic and highlights the way in which basic/translational research can inform clinical practice in an academic lipid clinic.
(1).jpg)
In the UCSD Lipid Clinic, we also evaluate and manage rare lipid disorders (e.g. homozygous familial hypercholesterolemia and beta-sitosterolemia), and frequently perform genetic testing for a variety of inherited lipid disorders. In many academic lipid clinics, including the program at UCSD, clinical observations inform research. Unique cases and clinical experiences (such as with implementation of new lipid-lowering therapies) lead to research questions and publications to advance knowledge in the field of lipidology.
Like many academic lipid treatment programs, the UCSD Lipid Clinic is located in a large city and functions as a referral center. Many referrals are internal (for example, from UCSD primary care physicians), but we also receive referrals from throughout San Diego County and beyond (with an especially wide geographic range of referrals from patients seeking special expertise in lipoprotein(a)). UCSD has the only lipoprotein apheresis unit in San Diego County, led by Dr. Amber Sanchez. We receive referrals to evaluate patients for lipoprotein apheresis, primarily from Southern California but occasionally from further abroad. We are fortunate to be able to offer this service, as lipoprotein apheresis centers are not accessible to patients in many parts of the United States.
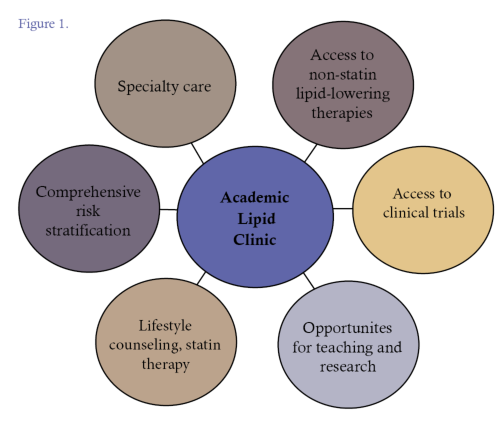
The Lipid Clinic at UCSD is made up of several faculty members with diverse interests and expertise to address multiple aspects of CVD prevention and lipid disorders; the program has grown considerably since 2018, and CVD prevention is also a focus of the Cardiac Rehabilitation and Wellness Center directed by Dr. Pam Taub. The focus, or purpose, of an academic lipid clinic, or preventive cardiology clinic, has been described by leaders in this growing field.2-4 The purpose of the Advanced Lipid Disorders Clinic at UCSD spans from research to clinical services, education and training both in Clinical Lipidology and CVD prevention (Figure 1). While academic lipid clinics and preventive cardiology clinics vary in size, scope, and structure, all are pushing boundaries in the field by advancing our understanding of lipid disorders and improving the lives of patients through early detection and treatment of preventable diseases, especially ASCVD.
Dr. Elizabeth Urteaga, Pharmacist, Primary care, Veterans Affairs
The Veterans Health Administration is the Nation’s largest health care system, with over 1,200 facilities serving over 9 million Veterans. The VA’s mission revolves around “I CARE” which stands for integrity, commitment, advocacy, respect, and excellence.5 Each Veteran is assigned to a Patient Aligned Care Team (PACT) for patient-centered, team-based primary care. Clinical pharmacists are embedded in primary care, often with one clinical pharmacist providing care for three PACT teams, or approximately 3,600 veterans. Clinical pharmacists with a specified scope of practice serve as medication experts to support primary care. This allows clinical pharmacists to function at a high level of autonomy, independently making decisions. It includes medication prescriptive authority ensuring that the most frequent drug-related management needs of patients with defined diagnoses are addressed, along with review of medication-related adverse events.

Our clinic schedules are built with 20-30 minute blocks for in-person visits and video telehealth visits. Regarding lipid management, I am frequently referred patients with hypertriglyceridemia and statin intolerance, but patients’ adherence to medication is also addressed. Medications are not always taken as prescribed, especially for chronic illnesses. Poor adherence is associated with increased morbidity and mortality and significantly contributes to health care costs. Interventions to improve medication adherence include patient education, medication regimen management, clinical pharmacist consultation for chronic disease management, cognitive behavioral therapies, and medication-taking reminders.7 One way I show “I CARE” every day is by explaining the importance of statin therapy to improve adherence. I push boundaries by implementing the NLA scientific statement: “Statin Intolerance: A New Definition and Key Considerations for ASCVD Risk Reduction in the Statin Intolerant Patient”.8 My time is focused on identifying and correcting modifiable factors associated with statin intolerance, working with patients to identify an acceptable statin treatment regimen, or in true statin intolerance, provide evidence-based non-statin therapies that have been shown to reduce adverse cardiovascular events. By following these steps, I again use the principles of “I CARE” and provide medications with a goal of lowering my patients’ risk for ASCVD events.
Ms. Elizabeth Jackson, Clinical Nurse Specialist, Lipid Specialist, Private Practice
Cardio Texas PLLC is an interventional cardiology group that serves both acute care and outpatient clinical settings. Located in Austin, Texas, I see a spectrum of patients from rural and urban settings, and with a wide range of health literacy. There is an art related to establishing a connection with each patient. It is essential to “meet the patient where they are” and have meaningful communication that enables them to make the best decisions regarding their health. Becoming certified as a Lipid Specialist in 2007 provided a career boost and enabled me to create an important niche within a very busy cardiology practice. An advanced practice provider with a specialty certification is perfectly positioned to ensure best practices and allow the physicians to focus on other aspects of patient care. In medicine, we must work around hurdles including cost, time, local availability, misinformation, quality metrics, and formularies/payer restrictions. For example, I do not have access to apheresis without sending patients to Houston or Dallas and have done so in the past. My patient population is generally well-served with the growing list of oral and injectable lipid-lowering options available from the pharmacy.
Limitations are imposed by inpatient formulary options which thus renders outpatient follow-up paramount. Lipids are assessed in any acute coronary syndrome admission, but lipids are also known to be lower in acute illnesses including myocardial infarction (MI), trauma, and malignancy. Total cholesterol may drop significantly in the early stages of acute illness.9 Thus, the lab result may not reflect true baseline lipid levels. In the setting of discharge following myocardial infarction, patients are prescribed high-intensity statin, and it is imperative to assess efficacy during follow-up; this is true any time we implement therapies, whether it relates to a lifestyle or pharmaceutical intervention. If we do not monitor response to therapy, we cannot ensure we are following guideline-directed medical therapy. Following the response to statin therapy after acute MI ensures that we are capturing accurate lipid values and obtaining the expected lipid-lowering response to therapy. This is a very important aspect of my outpatient practice. I am always looking for opportunities to push the boundaries in order to optimally treat, assess treatment efficacy, and alter strategies as needed.

Guidelines are written to offer evidence-based therapeutic direction for individual patients and include lifestyle management as the foundation of care with additional medical options as appropriate in primary and secondary prevention of cardiovascular disease and in patients with FH.10,11 Addressing lifestyle with every patient at every visit is essential in their care. Challenges with lifestyle counseling in practice are limited by time and resources, such as lack of access to dietitians or exercise physiologists beyond those involved in cardiac rehabilitation programs. Simply asking about a patient’s dietary habits and physical activity places emphasis on the importance of making lifestyle the foundation of treatment. However, the depth of knowledge and availability of resources at the patient level varies greatly and likely requires more time than allotted at their appointment. One method of pushing the boundaries by ensuring lifestyle is the foundation of treatment is through shared medical appointments (SMA) that can generally include up to 12 patients. This allows peer interaction as well as consistent dissemination of information. This format also directly addresses challenges by, “improving access to care, reducing cost to patients and hospitals, reducing provider burnout and improving clinical outcomes.”12 SMA offers efficient delivery of care, the benefit of patients learning from each other while allowing billing at usual office visit levels (level 99212, 99213, or 99214). We are currently working to implement this structure in our practice, thus pushing the boundaries with creative and productive patient visits.
Ms. Lauren Williams, Registered Dietitian, Pediatric Lipid Clinic
The Risk Evaluation to Achieve Cardiovascular Health (REACH) Clinic is a pediatric lipid clinic housed in the Department of Endocrinology and Diabetes at Cook Children’s Medical Center in Fort Worth, Texas. As a specialty clinic located within an urban setting, the REACH Clinic receives referrals from primary care providers in the surrounding area as well as from other specialties and satellite clinics within the Cook Children’s network. Our team includes 2 physicians, 2 nurses, a dietitian, research coordinator, as well as shared medical assistants, a clinical pharmacist, social worker, nurse practitioners, and clinical therapists within the Department of Endocrinology. Patients receive nutrition counseling at each clinic visit, and we work together to provide patient-centered care and fulfill Cook Children’s pinky promise of, “Everything for the child.” Sometimes, this means nutrition education, or it may include a referral to our clinical therapy team to help patients overcome any psychosocial barriers to change.

In an effort to identify patients with familial hypercholesterolemia, the REACH Clinic partnered with Cook Children’s neighborhood clinics to offer routine point-of-care lipid screening at each 2-year-old well-child visit. This screening is based on findings by Wald, et al., which showed the feasibility and efficacy of screening for familial hypercholesterolemia in the primary care setting at 1-2 years of age.13
Our clinic is also pushing boundaries by offering genetic testing for patients with presumed familial hypercholesterolemia or familial chylomicronemia syndrome, and by using reverse cascade screening to identify any family members who also may have elevated lipid levels.
As a pediatric lipid dietitian, there are many barriers to overcome in order to provide the best care for patients. There are a limited number of pediatric-specific publications or guidelines, particularly a limited number of pediatric-specific nutrition studies/publications. Often, we must extrapolate data from adult studies to fit the pediatric population. There are also very few publications regarding the use of nutrition supplements in children.
Another challenge is a lack of insurance coverage for nutrition counseling. Often insurance will only pay for RD visits if a patient has diabetes or nephrotic syndrome. Lack of coverage often leads to the patients with private insurance incurring a charge for RD services, and conversely some patients opt to forego RD counseling altogether. In the REACH Clinic, we are pushing past this barrier with the help of the medical center’s generosity as they provide funding to help cover the RD’s role.
Within the NLA, I’ve been pleased to see a growing number of individuals working with pediatric patients. According to most recent numbers, the NLA includes 148 individuals who self-identify as specializing in pediatrics, 37 specializing in pediatric endocrinology, and 42 specializing in pediatric cardiology. I hope to see this small, but mighty group continue to help our small, but mighty patients!
Not to be overlooked is the other small, but mighty group of 37 dietitians who are currently members of the NLA. We continue to push forward to provide medical nutrition therapy to patients as well as nutrition resources, such as the NLA’s Clinical Lifestyle Modification Toolbox (CLMT) tear sheets.14
Conclusions
“If you do not push the boundaries, you will never know where they are.” - T.S. Elliot
While lipid specialists are diverse in their background, training, and practice settings, we all share the common goal of helping patients to live healthier lives and reduce the risk of cardiovascular disease. We employ our varied and complementary strengths in facing these challenges. We look forward to continued growth in the field of clinical lipidology as more healthcare professionals contribute to achievement of providing a comprehensive network of services for diverse patients across urban, suburban, and rural environments. We need more professionals with expertise in lipidology and CVD prevention to push boundaries, broaden access to services, and reach a greater number of patients.
Dr. Wilkinson has received research support from Amgen, and consulting fees from Amarin, Regeneron, and The Kinetix Group. Dr. Urteaga has no financial relationships to disclose. Ms. Jackson has received honoraria from Novartis, Esperion, and Regeneron. Ms. Williams has no financial relationships to disclose.
References
- Tsimikas S, Stroes ESG. The dedicated “Lp(a) clinic”: A concept whose time has arrived? Atherosclerosis 2020;300:1-9.
- Shapiro MD, Maron DJ, Morris PB, et al. Preventive Cardiology as a Subspecialty of Cardiovascular Medicine: JACC Council Perspectives. Journal of the American College of Cardiology 2019;74:1926-42.
- Liebeskind A, Warden BA, Sikand G, Duell PB, Guyton JR. JCL Roundtable: Lipid clinic operations. Journal of clinical lipidology 2019;13:511-21.
- German CA, Baum SJ, Ferdinand KC, et al. Defining preventive cardiology: A clinical practice statement from the American Society for Preventive Cardiology. Am J Prev Cardiol 2022;12:100432.
- Pharmacists. Updated August 7, 2022. Accessed December 1, 2022, at https://www.vacareers.va.gov/careers/pharmacists/#health-care-system.)
- VHA Handbook 1108.11(1). Clinical Pharmacy Services. July 1, 2015. Accessed December 1, 2022, at https://www.va.gov/vhapublications/publications.cfm?Pub=2.)
- Kini V, Ho PM. Interventions to Improve Medication Adherence: A Review. JAMA : the journal of the American Medical Association 2018;320:2461-73.
- Cheeley MK, Saseen JJ, Agarwala A, et al. NLA scientific statement on statin intolerance: a new definition and key considerations for ASCVD risk reduction in the statin intolerant patient. Journal of clinical lipidology 2022;16:361-75.
- Luthold S, Berneis K, Bady P, Muller B. Effects of infectious disease on plasma lipids and their diagnostic significance in critical illness. Eur J Clin Invest 2007;37:573-9.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;140:e596-e646.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019;139:e1082-e143.
- Lacagnina S, Tips J, Pauly K, Cara K, Karlsen M. Lifestyle Medicine Shared Medical Appointments. American Journal of Lifestyle Medicine. July 2020; 15:1, 23-27
- Wald DS, Bestwick JP, Morris JK, Whyte K, Jenkins L, Wald NJ. Child-Parent Familial Hypercholesterolemia Screening in Primary Care. N Engl J Med 2016;375:1628-37.
- National Lipid Association (NLA) Clinician’s Lifestyle Modification Toolbox. (Accessed January 3, 2023, at https://www.lipid.org/clmt)
Article By:
Assistant Professor of Medicine
Director, Lipid Clinic
Division of Cardiovascular Medicine, Department of Medicine
Cardiovascular Institute
University of California San Diego
San Diego, CA
Cardio Texas, PLLC
St. David’s Medical Center
Austin, TX
Clinical Pharmacy Specialist Practitioner, PACT
South Texas Veterans Health Care System
San Antonio, TX
Clinical Dietitian II
Endocrinology and Diabetes Clinic
Cook Children’s Medical Center
Fort Worth, TX





.jpg)
.png)










