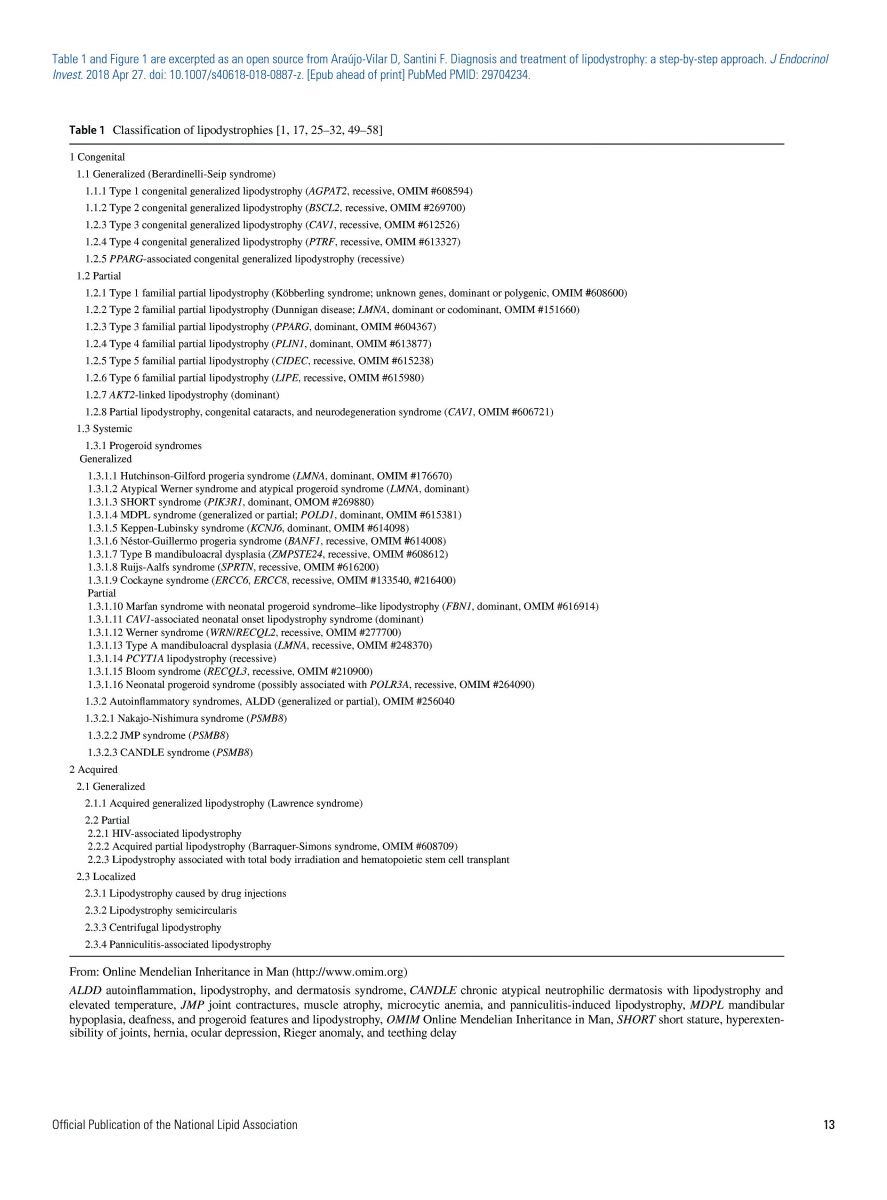
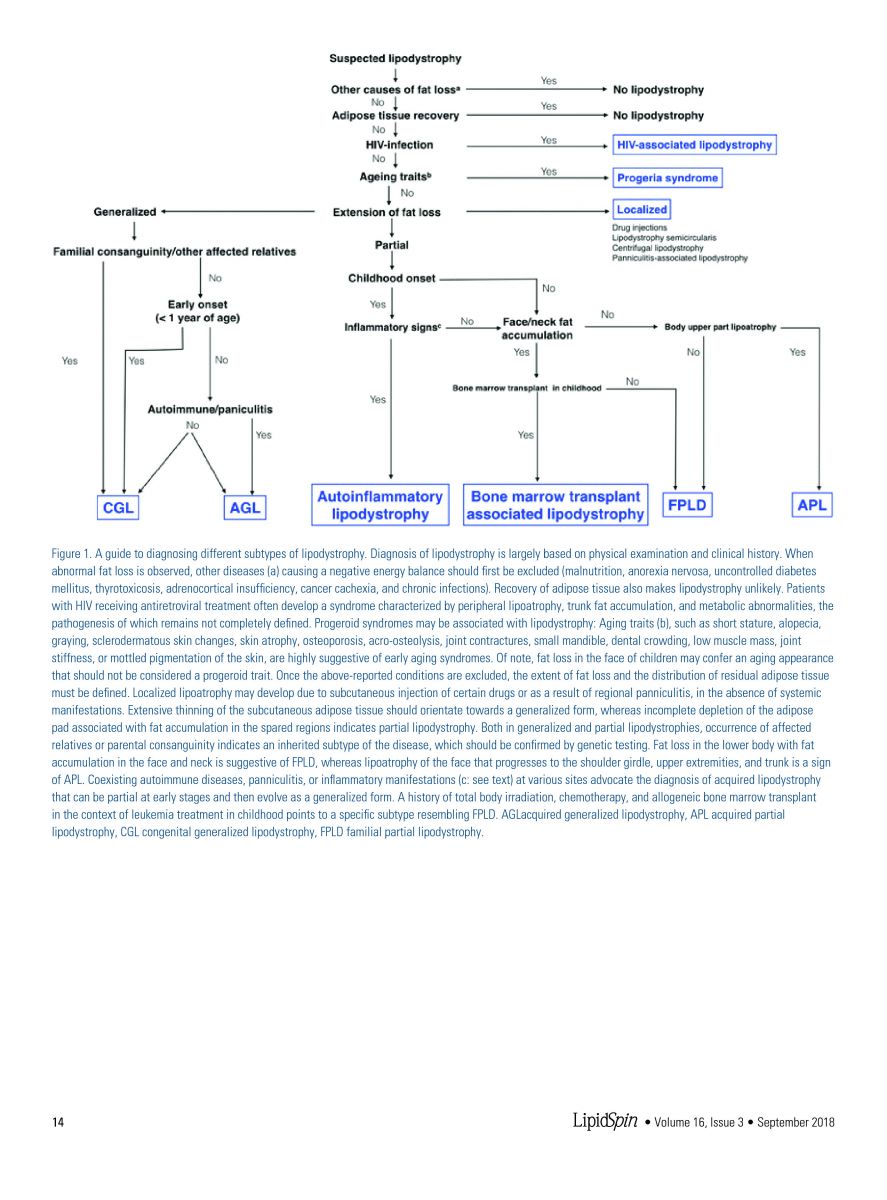
Lipodystrophies are a group of disorders of fat tissue loss that are classified according to whether the condition is genetic or acquired and by the distribution of fat loss, either generalized or partial (Table 1).1 Generalized lipodystrophy is a rare, complex, and clinically heterogeneous disorder characterized by the widespread loss of adipose tissue. Patients appear lean and muscular because muscle definition is often obvious due to absence of subcutaneous fat. Counterintuitively, the metabolic sequelae of this lipodystrophy subtype are often the most severe. Lipodystrophy is often associated with premature mortality due to cardiovascular disease, liver disease, kidney failure, pancreatitis, and/or sepsis. Other comorbidities may accompany this condition as well. This includes physical disfigurement and associated psychosocial stress, peripheral neuropathy, foot and other skin infections due to neuropathy, loss of fat pad on both feet, and inconsolable hunger in the case of generalized lipodystrophy with absent leptin. Because the rarity of certain subtypes, lipodystrophy may frequently go unrecognized.2 Araújo-Vilar and Santini have described the clinical presentation of known types of lipodystrophy and organized them into a diagnostic algorithm. (Figure 1).1 Fortunately, genes associated with many congenital forms of lipodystrophy have been identified and genetic testing may assist both in confirming the diagnosis of lipodystrophy and in identifying the subtype of this disorder.
Treatment of patients with lipodystrophies should include a healthy low-fat high-fiber diet with complex carbohydrates, regular activity, and management of comorbidities per current evidence-based standards of care.3 To minimize hypertriglyceridemia, dietary fat should not exceed 30% and medium-chain triglyceride-based formulas should be used in infants. Of the fats consumed, cis-monounsaturated and long-chain omega-3 fatty acids are recommended for all ages. When hypertriglyceridemia is severe (>2000 mg/dL) or results in chylomicronemia syndrome, very low–fat diets (<15-20%) should be instituted, although this may be difficult to manage particularly during adolescence. Part 2 NLA recommendations suggest that the diet should contain <15% total fat to adequately clear chylomicrons. Patients may have a history of multiple hospitalizations for chylomicronemia associated pancreatitis, and often an enlarged fatty liver is present with non-alcoholic steatohepatitis. There are no known treatments to treat hepatic steatosis or steatohepatitis associated with lipodystrophy.1,2 During hospitalization for acute pancreatitis, oral food should be withheld until circulating chylomicrons are cleared and triglyceride levels return to <1000 mg/dL. In children with lipodystrophies, growth assessment may be challenging because of the abnormal body composition and linear growth may be independently affected by the underlying primary disease that triggers the expression of lipodystrophy. Physical exercise as tolerated and tailored to adapt with coexisting physical conditions is recommended. Psychosocial support is essential. Selective plastic surgery under certain conditions may be helpful.
Lipid lowering drugs should be used for those patients yet to reach goal after diet and lifestyle intervention in keeping with Part 2 NLA recommendations. When present, diabetes control will also be key to recovery. Patients with insulin resistance and diabetes mellitus should be treated with conventional therapies, including oral agents where metformin is the first-line agent and insulin. Insulin therapy often provides the mainstay of treatment because of severe insulin resistance and many patients require concentrated forms such as 500 U regular insulin. Type 2 diabetes may be difficult to control despite high-doses of insulin. Sub-cutaneous injections are often problematic because of discomfort in patients with generalized lipodystrophy because of paucity of subcutaneous fat stores. Uncontrolled hypertension may be treated with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers to control proteinuria.
Most of these sequelae are thought to be due to the ectopic deposition of triglyceride in liver and muscle that occurs when subcutaneous depots are unavailable for storage. As previously mentioned, leptin levels are very low when adipose tissue is absent in a generalized distribution. Leptin’s action in peripheral tissues includes enhancing fat oxidation. Both animal and human trials of leptin replacement in these patients showed remarkable reductions in liver fat accompanied by improvements in hyperglycemia and hypertriglyceridemia.1,3,4
In addition to management recommendations for comorbid conditions, lipodystrophy patients also have newer a treatment option. Metreleptin is a leptin analog approved in 2014 by the FDA as an adjunct to diet and other supportive therapy to treat the complications of leptin deficiency in patients with congenital or acquired generalized lipodystrophy, but not for partial lipodystrophy or for acquired HIV-related lipodystrophy.5 Currently, metreleptin is not indicated for treatment of other metabolic disease without the diagnosis of generalized lipodystrophy or of liver disease, including nonalcoholic steatohepatitis (NASH). Rarely, anti-metreleptin antibodies may form and inhibit action of any endogenous leptin and of metreleptin itself. In such cases, worsening metabolic control and severe infection have been reported.5
In summary, lipodystrophies are a rare but important group of disorders for lipidologists to consider in patients with moderate to severe hypertriglyceridemia when it is accompanied by severe insulin resistance, ie, diabetes requiring doses of insulin often far greater than 100 units per day. This particularly holds true when patients present with a lean phenotype. Generalized lipodystrophy must be distinguished from familial chylomicronemia syndrome (FCS) in which TG levels are often much higher (1,000 to 10,000 mg/dL or higher) and not responsive to TG-lowering medications (fibrates, prescription omega-3, niacin or statins).6 FCS patients can be slender or overweight/obese, but adipose tissue will be visible in the extremities. Testing for mutations in genes related to lipodystrophy and/or FCS may help distinguish these diseases. Treatment for the lipodystrophies includes intensive lifestyle management, proper diabetes control and TG-lowering medications, and in the case of generalized lipodystrophy with low leptin levels, replacement with metreleptin.
Disclosure statement: Dr. Purnell serves on the advisory board of Nono Nordisk. Dr. Brinton has received honoraria from Amarin, Amgen, Alexion, Janssen, Boehringer, Kastle, Kowa, Merck, Rengeron, Novo Nordisk and Sanofi. Dr. Fazio has served as an ad hoc consultant for Amgen, Aegerion, Akcea, Amarin, and Kowa. Dr. Neff has no disclosures to report.
References can be found here.
Article By:
The William and Sonja Connor Chair of Preventive Cardiology
Professor of Medicine and Physiology & Pharmacology
Director, Center for Preventive Cardiology
Knight Cardiovascular Institute
Oregon Health & Science University
Portland, OR
Diplomate, American Board of Clinical Lipidology





.jpg)
.png)