Background
In the United States, hypertension accounts for more cardiovascular disease (CVD) deaths than any other modifiable CVD risk factor and is second only to cigarette smoking as a preventable cause of death. In 2010, high blood pressure (BP) was the leading cause of death and disability worldwide. Although hypertension remains the most common modifiable risk factor for CVD, a large portion of the population still has BP that remains uncontrolled.
New guideline definitions
Until the recent 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults(1), it had been more than 20 years since the last updated classification of BP. Based on the new guideline, “normal BP” still is defined as < 120/80 mmHg but gone is the term “pre-hypertension” which was used in the 7th Joint National Committee Report of 2003. Instead, “elevated blood pressure” is defined as a systolic pressure between 120-129 mmHg and a diastolic pressure < 80mmHg. (Figure 1). “Stage 1 hypertension” now is defined as a systolic BP between 130-139 mmHg or diastolic BP between 80-89 mmHg. “Stage 2 hypertension” is defined as a systolic BP ≥ 140 mmHg or diastolic ≥ 90mmHg. This classification is based on an average of two or more careful readings obtained on two or more occasions. Using the new classification and based on 2011-2014 data from the National Health and Examination Survey (NHANES), it is projected that the prevalence of hypertension will increase from 34% to 46%, increasing the number of hypertensive people from 72 million to 103 million. However, the percentage of hypertensive people new to pharmacologic treatment will increase only from 34.3% to 36.2%. This increases the number of new of patients recommended for drug therapy by 4.4 million in the U.S. (77.7 million to 81.9 million).(2) The majority of patients with newly diagnosed Stage 1 hypertension, especially those under 45 years of age, may be candidates for nonpharmacological therapy with lifestyle modification alone and no drug therapy.
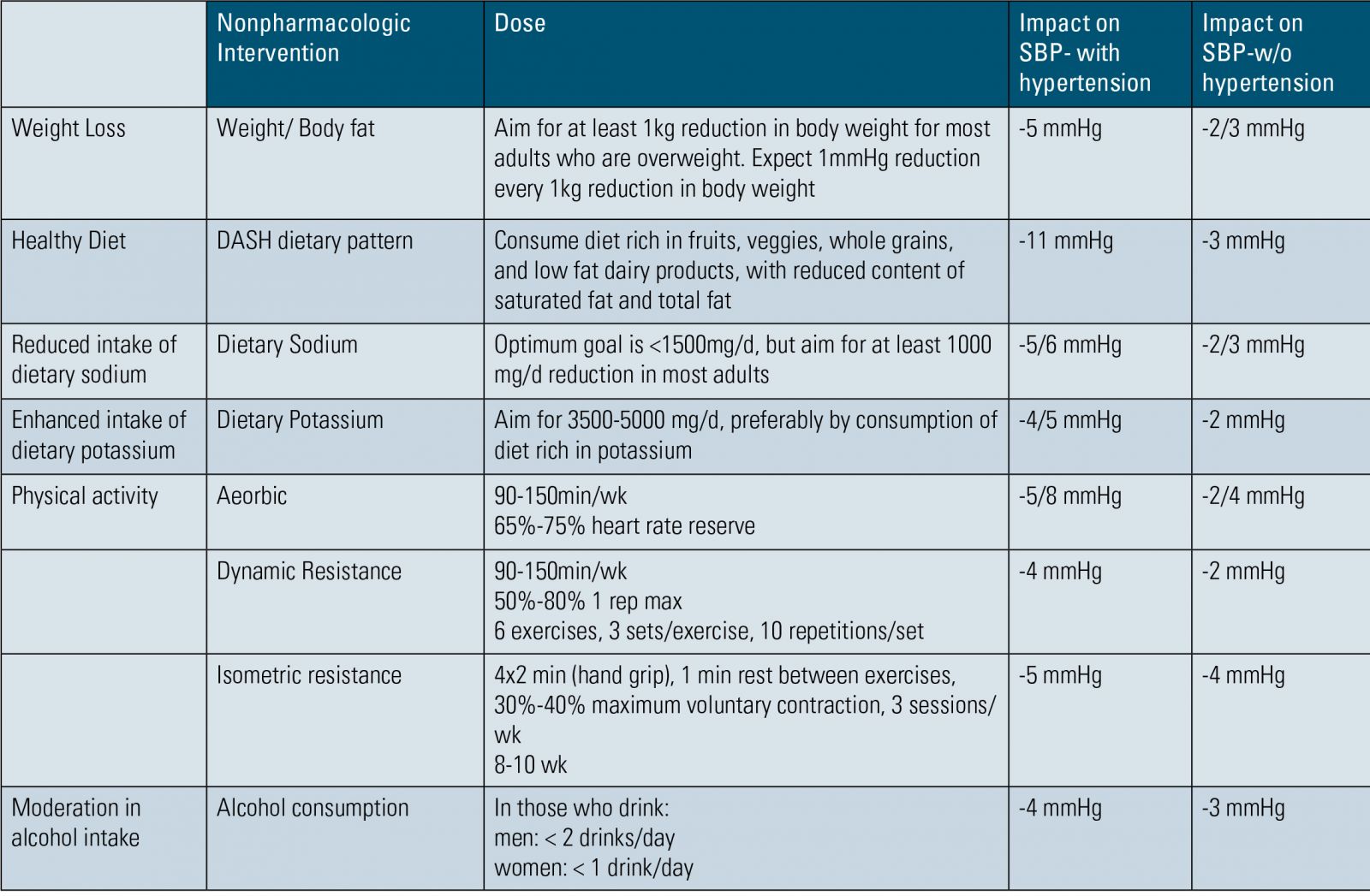
Table 1.
Evaluation of hypertension
In newly diagnosed hypertension, it is important to evaluate the patient’s dietary habits, sodium intake, physical activity and alcohol and tobacco use. Patients also should undergo basic laboratory testing, which includes fasting blood glucose; complete blood count (CBC); lipid profile; serum creatinine with estimated glomerular filtration rate (eGFR); serum potassium, sodium and calcium; thyroidstimulating hormone levels; urinalysis; and electrocardiogram. Optional testing includes echocardiogram, serum uric acid and urinary albumin-to-creatinine ratio. These tests may provide additional information pertaining to organ damage. The goal of evaluation is to identify potential secondary causes of hypertension and the presence of end organ damage, and to tailor an appropriate treatment regimen. Hypertension associated with weight gain, modifiable lifestyle factors, decreased physical activity or advancing age in a patient with a strong family history of high blood pressure points toward primary hypertension as the likely diagnosis. In the setting of clinical features suggesting possible secondary causes of hypertension – pheochromocytoma, obstructive sleep apnea, chronic kidney disease, primary aldosteronism, Cushing’s syndrome, medication or substance use – additional diagnostic evaluation may be indicated.
Blood pressure monitoring
The 2017 ACC/AHA BP guideline recommends that office BP measurement be used primarily in screening for possible hypertension. In an effort is avoid misclassifying patients who actually may have white coat hypertension, it is recommended that out-of-office BP should be used to confirm the diagnosis of hypertension and for monitoring response to therapy and medication titration. Home BP monitoring using proper measurement techniques and validated devices should be recommended. There are a number of oscillometric devices that have been validated for accuracy for home use (bihsoc.org/bp-monitors) and it is helpful to
provide patients with guidance on device selection (validated devices, use-arm [not wrist] devices, use of proper cuff size and proper measurement technique). There is a trend toward recommendations for the use of automated oscillometric devices in the office setting rather than an aneroid device with stethoscope, as was used in the Systolic Blood Pressure Intervention Trial (SPRINT) and in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) BP outcome studies.
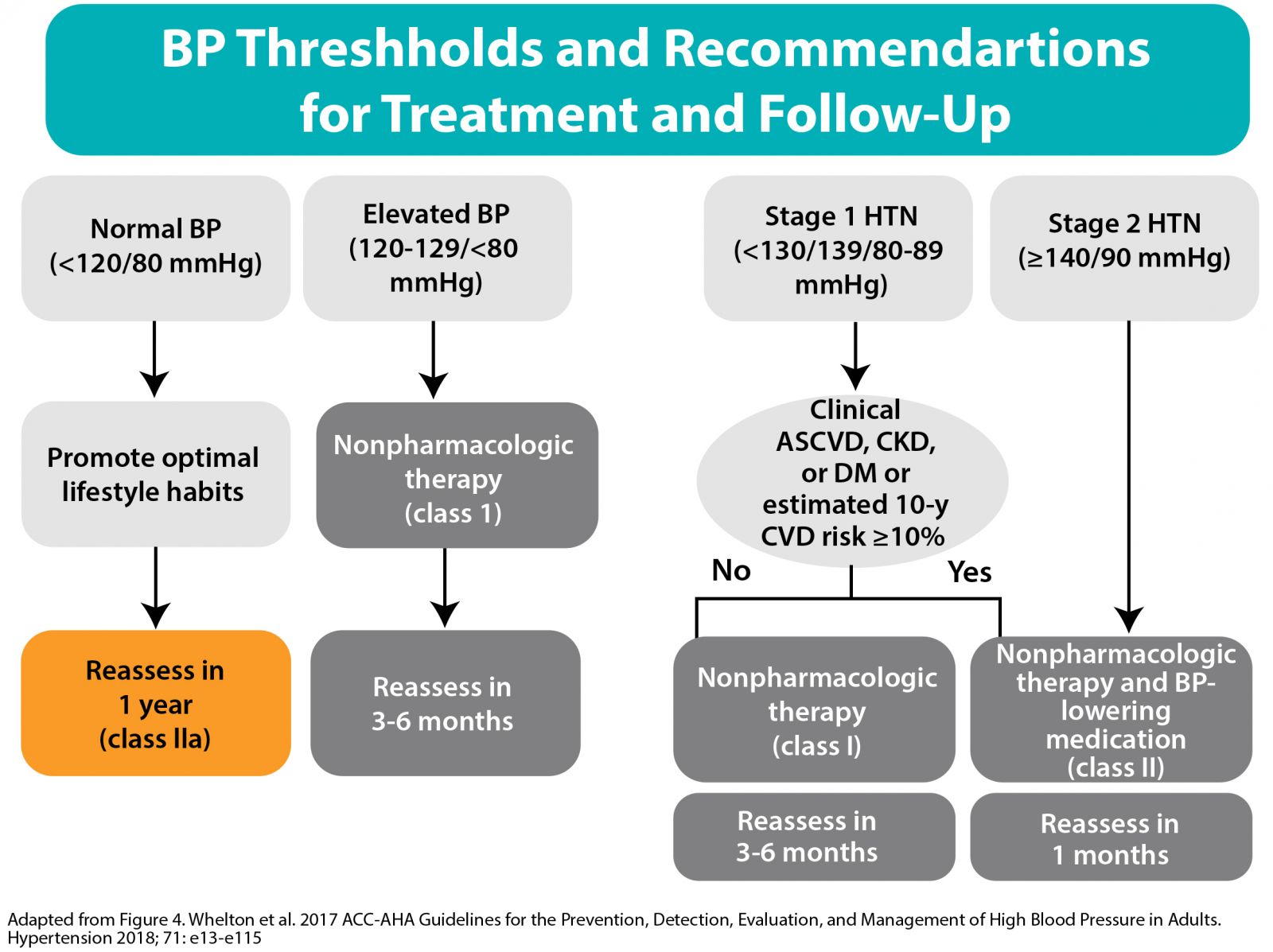
Adapted from Figure 4. Whelton et al. 2017 ACC-AHA Guidelines for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. Hypertension 2018; 71: e13-e115
Figure 2.
TREATMENT OF HYPERTENSION
Lifestyle modifications
Lifestyle modification alone is a Class I recommendation for those with elevated BP and Stage 1 hypertension with low (<10%) atherosclerosis cardiovascular disease (ASCVD) risk and in all those requiring antihypertensive drug therapy. The following are Class IA recommendations for nonpharmacological interventions in reducing BP: weight loss (when appropriate); adherence to a heart-healthy diet, such as the Dietary Approaches to Stop Hypertension (DASH) diet; sodium reduction; potassium supplementation (unless contraindicated by the presence of chronic kidney disease or hyperkalemia); increased physical activity; and limiting alcohol consumption to no more than 1 or 2 drinks a day for women and men, respectively (Table 1). These nonpharmacologic interventions may be sufficient to prevent hypertension or achieve goal BP levels for those with Stage 1 hypertension.
Pharmacologic therapy for Stage 1 hypertension
For patients with Stage 1 hypertension, pharmacologic therapy is recommended in addition to lifestyle modification if patients have a history of ASCVD, diabetes, chronic kidney disease (CKD); 10-year predicted ASCVD risk > 10%; or age > 65. All patients with Stage 2 hypertension should be initiated on pharmacologic antihypertensive therapy in addition to lifestyle modification (Figure 2).





.jpg)
.png)












