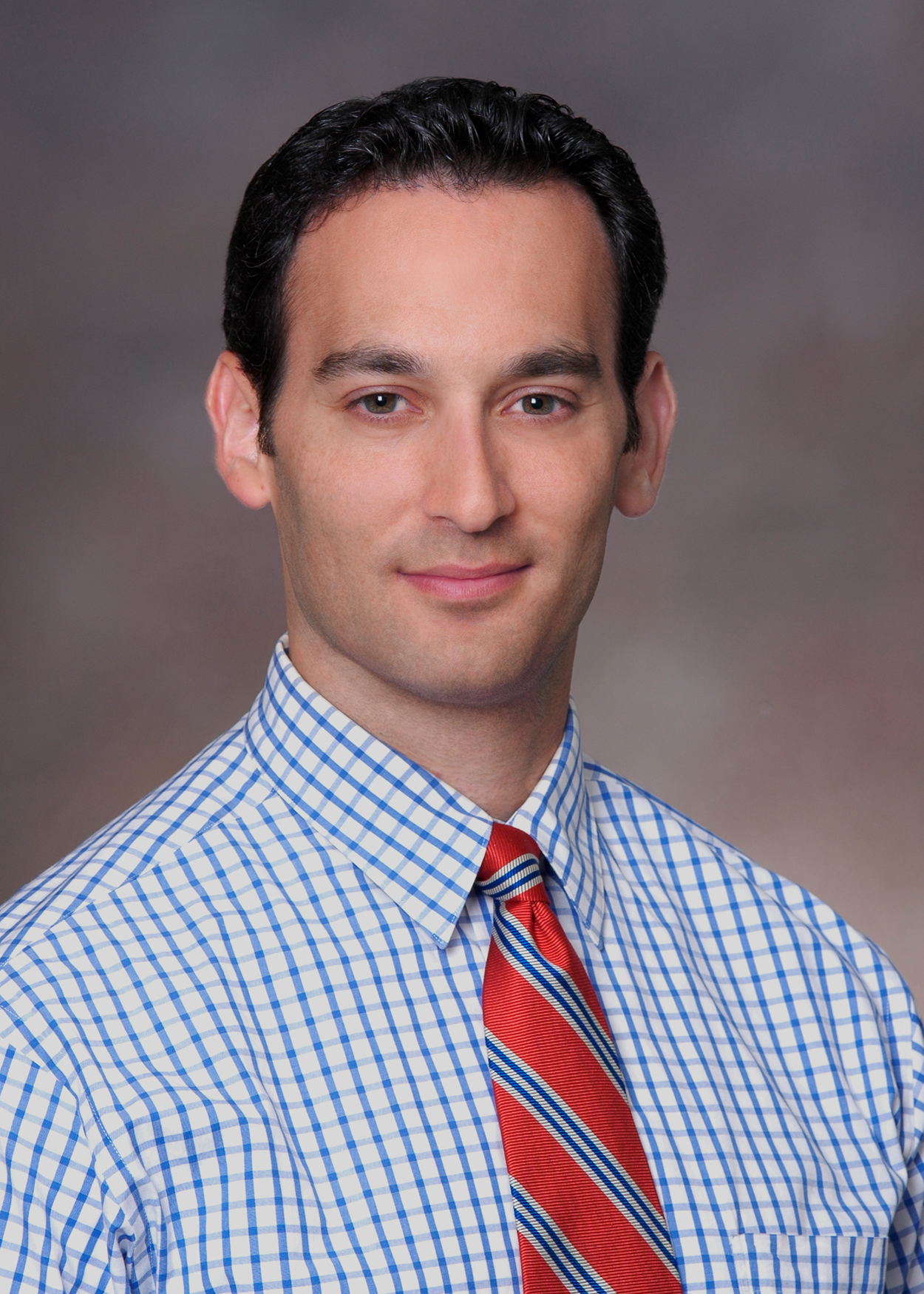
Atherosclerotic cardiovascular disease (ASCVD) is the major cause of morbidity, mortality, and medical costs in the U.S. While ASCVD is largely preventable with a healthy lifestyle and effective medical therapy, identification of individuals at risk for ASCVD events continues to be a challenge. Historically, the Framingham Risk Score (FRS)1 and now, the Pooled Cohort Risk Equation,2 are used to estimate 10-year risk of coronary heart disease (CHD) and ASCVD, respectively, and are incorporated into cholesterol treatment guidelines.3,4 Unfortunately, many patients experiencing ASCVD are not classified as high risk by such approaches.5 The role of biomarkers and imaging tools has been of interest to those trying to improve risk stratification of asymptomatic individuals. One of the most promising such modalities is coronary calcium scanning by computed tomography (CT); the coronary artery calcium score (CACS) (Figure1) estimates subclinical atherosclerotic burden. The theoretical framework for CACS is based on autopsy studies that consistently demonstrate a unique association between calcification of the coronary arteries and atherosclerosis.6
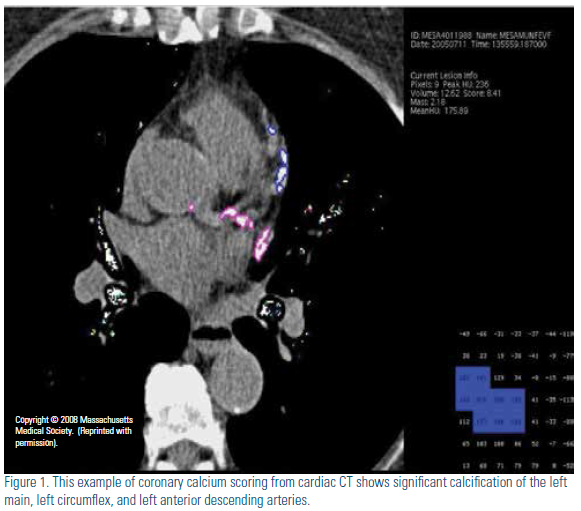
CACS and Prognosis The prognostic value of CACS is clearly established from a wealth of prospective studies performed in tens of thousands of patients, with strong associations found with ASCVD events and mortality.7-10 Among the largest, the Multi-Ethnic Study of Atherosclerosis (MESA) study7 enrolled 6,722 black, Hispanic, Chinese, and white participants. The four-year follow-up of this cohort demonstrated that, compared to individuals with a CACS of 0, those with CACS 1-100 had a 3.9-fold and those with a CACS >100 a 7.1-fold greater risk of CHD events. Also, a normal scan (score of 0) is considered to indicate a “warranty period” of up to five years free from developing future CHD events.
CACS and Prognosis
The prognostic value of CACS is clearly established from a wealth of prospective studies performed in tens of thousands of patients, with strong associations found with ASCVD events and mortality.7-10 Among the largest, the Multi-Ethnic Study of Atherosclerosis (MESA) study7 enrolled 6,722 black, Hispanic, Chinese, and white participants. The four-year follow-up of this cohort demonstrated that, compared to individuals with a CACS of 0, those with CACS 1-100 had a 3.9-fold and those with a CACS >100 a 7.1-fold greater risk of CHD events. Also, a normal scan (score of 0) is considered to indicate a “warranty period” of up to five years free from developing future CHD events.11
CACS Provides Added Clinical Utility over Global Risk Assessment
Improved discrimination from adding information from CACS can be shown from measures such as the C-statistic, based on the area under the receiver operating characteristic (ROC) curve, which evaluates the overall performance of the risk model. MESA and other prospective studies have demonstrated improvements in the C-statistic over standard risk factors and/or FRS. Notably, MESA confirmed the incremental value of CACS for predicting CHD events to be consistent across all ethnic groups.7 However, many advocate the use of the net reclassification index (NRI), which quantifies the clinical utility of a diagnostic test, although —importantly — the NRI depends on the cut points chosen (e.g., for classification of risk category based on 10-year risk of CHD). The NRI is a measure of the appropriate upgrading or downgrading of risk based on the new information provided by a diagnostic test, in this case CACS. Three large trials of distinct populations have shown a significant improvement in the NRI when using CACS to refine risk estimates. In the MESA study, the NRI for the entire population was 25 percent. However, when focusing on the intermediate risk population (the population in which CACS testing is proposed) the NRI increased to 55 percent.12 The Heinz Nixdorf Recall study found that use of CACS in subjects classified as low-intermediate risk (6 to 20 percent) based on FRS led to reclassification of 31 percent of subjects.13 Additionally, the Rotterdam study demonstrated an NRI of 52 percent in subjects in the intermediate risk group (in this case 10 to 20 percent by FRS).14 Overall, the NRI based on CACS in riskstratification is substantial, particularly in those at intermediate risk, and help define which patients need more aggressive medical management.
The Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER trial) demonstrated that those with a lowdensity lipoprotein cholesterol (LDL-C) <130 mg/dL but high-sensitivity C-reactive protein (hsCRP) ≥2 mg/L may benefit from treatment with rosuvastatin.15 In an analysis from MESA,16 950 subjects were found to meet the JUPITER criteria. Interestingly, almost half of those identified had a CACS of 0. Applying JUPITER eventreduction estimates, statin treatment would likely be neither clinically effective nor cost effective (number needed to treat [NNT] = 549). In contrast, most events (74 percent) occurred in individuals with CACS > 100 and, in this group, statin treatment was estimated to be highly effective (NNT = 24). More recently, even greater “efficacy” for prevention of CHD events was shown when applying results of recent polypill trials to MESA, with NNTs of 18-20 for those with CACS >100 and 38-54 for those with CACS of 1-99, but not in those with CACS = 0 (NNTs 81-130).17 Thus, CACS appears to have significant utility in identifying those most likely to benefit from preventive therapies.
CACS Compared to other Screening Tests
The most robust evidence comparing the utility of CACS to other screening tests derives from Yeboah, et al.,18 where a direct comparison of the improvement in risk prediction was made using several different biomarkers and screening tests among intermediate risk subjects in MESA. Ankle-brachial index, hsCRP, family history and CACS were all independent risk predictors for incident CHD and ASCVD (brachial flow-mediated dilation and carotid intima-media thickness were not) over FRS and provided significant improvements in C-statistic over FRS alone. However, CACS provided superior risk reclassification compared with the other risk markers. (For incident CHD, the NRI with CACS was 0.659, brachial flow-mediated dilation was 0.024, ankle-brachial index was 0.036, carotid intima-media thickness was 0.102, family history was 0.160 and highsensitivity CRP was 0.079).
Clinical Recommendations for Use of Coronary Calcium Scanning
On the basis of these consistent observations, the 2010 ACC/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults provided a class IIa recommendation for performance of CACS in intermediate-risk patients and in those aged 40 years and above with diabetes.19 Recent ACC/AHA Guidelines on the Assessment of Cardiovascular Risk also noted that CACS is likely to be the most useful screening test to improve risk assessment in those at intermediate risk2 and suggested consideration of CACS evaluation when a treatment decision based on global risk assessment is uncertain. The recent ACC/AHA blood cholesterol management guideline specifically notes that a CACS of >300 or >75th percentile for age, gender and ethnicity provides support to revise risk assessment upward and, hence, potentially inform treatment (initiation or intensification) decisions.4
Disclosure statement: Dr. Wong has received salary through his institution from Amgen, Bristol-Myers Squibb, Gilead, and Regeneron. Dr. Wong has received consulting fees from Aviir and Amgen. Dr. Shapiro has received consulting fees from Aegerion and Isis Pharmaceuticals.
References are listed on page 35 of the PDF.






.jpg)
.png)