“An ounce of prevention is worth a pound of cure.” — Benjamin Franklin
Introduction
Truisms carry no scientific weight, but that doesn’t mean they can’t be true. For decades now, primary prevention has been based on the cardiovascular risk model. This approach, which appears simply to be common sense and therefore inarguable, was developed because clinical events are what injure or kill us and clinical events are, therefore, what we should aim to prevent. Those at higher risk, by definition, are more likely to suffer clinical events and, therefore, they should be the optimal candidates for primary prevention. We acknowledge that the concept of risk is powerful and has done much to improve care.
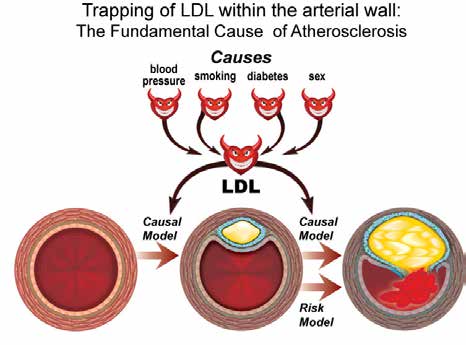
However, we will argue that this is an imperfect strategy in practice, which leads to less-than-optimal prevention. Indeed, as presently practiced, this strategy amounts too often to action after the fact rather than before the fact. By contrast, the model we support — the causal exposure model of vascular disease1 — aims to prevent the clinical event by first preventing the disease within the arteries that leads to the clinical event. We will argue that preventing retention of low- density lipoprotein (LDL) apolipoprotein B (apoB) particles within the endothelium of the arterial wall prevents the sentinel event that initiates, propagates, and helps to complete the intricate chain of reactions that over time produces complex pathologic lesions within the arterial wall.3 Therefore, we will argue that younger individuals with elevated levels of LDL should be treated earlier than called for by the conventional risk approach.1,2 Simply put, we will, argue that an ounce of prevention is indeed worth a pound of cure.
Limitations to the Conventional Risk Model of Cardiovascular Events for Primary Prevention of Cardiovascular Disease
While the details differ, almost all guidelines select candidates for primary prevention based on the calculated risk of a cardiovascular event over the next decade. This risk estimate is derived from a multiple regression algorithm incorporating age and a number of variables such as hypertension, lipids, smoking, gender, and diabetes. Except for those with extreme elevations of LDL and diabetes, only if the risk of a clinical event exceeds an arbitrary threshold is LDL-lowering therapy instituted. In this model, it is risk that matters, not the factors that create risk, because it is presumed that the benefit of LDL-lowering therapy is determined by risk, not by specific factors such as LDL. This model is so broadly accepted and so little debated that its limitations have largely escaped detection.
 Limitations to the Risk Prevention Model
Limitations to the Risk Prevention Model
1. Total benefit is limited once complex lesions are present. Clinical cardiovascular events are the result of any of a series of abrupt, calamitous, tectonic transformations within an arterial segment in which advanced, complex disease is present. These include plaque rupture, plaque fissure, intramural haemorrhage, and endothelial denudation.4-6 If prevention is triggered by risk and risk is the consequence of disease, it follows that prevention often only starts after extensive, advanced, complex disease is present. Starting LDL-lowering therapy at this point limits its effectiveness because only some of these pathophysiological catastrophes are preventable with statin therapy. Thus, statin therapy may well reduce the risk of plaque rupture but is unlikely to reduce the risk of intramural haemorrhage from neovascularization. Treating the causes before they irreversibly injure the arterial wall would seem a more prudent and a more effective prevention strategy.
2. Early events will not be prevented because age is the major determinant of the conventional estimate of risk.
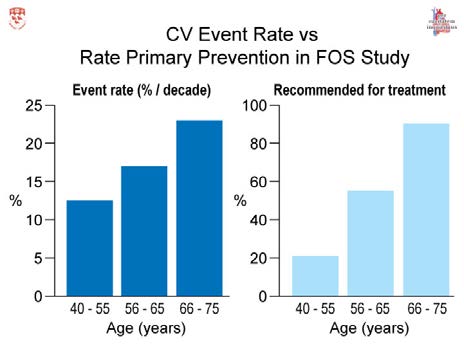
In any risk algorithm that projects risk for a decade, age and then gender are the overwhelming determinants of risk. Thus, the recent American College of Cardiology/ American Heart Association (ACC/AHA) guidelines make statin therapy the rule in those over 60 and the exception in those under 60.2 If the ACC/AHA guidelines are applied to the Framingham Heart Study population (Figure 1), 21 percent of those ages 40 to 55, 40 percent of those between 55 and 65, but more than 90 percent of those >65 would be eligible for primary prevention.7 The rate at which eligibility increases is much steeper than the age-related incidence of cardiovascular events, which is 12.5 percent over 10 years between ages 40 to 55 years; 19.3 percent between age 55 to 65 years; and 25 percent between ages 65 to 75 years.3 The high event rate at an early age contrasts with the low rate of preventive therapy at an early age; the slow steady increase in event rate contrasts with the eventual staggeringly high, indeed almost universal, rate of prescriptions for statins for the elderly.
Guidelines to the contrary, the incidence of cardiovascular events before age 65 and even before age 55 is, by any measure, substantial. Indeed, if the natural history of vascular disease were to be torn up and rewritten such that it starts at 40 and stops at 55, the murder and mayhem it would still cause — the massive number of individual tragedies, all the more calamitous before those affected were in their prime — would still be an exceedingly significant public health problem. Since prevention does not become common until after age 60,2 most of those who suffered a cardiovascular event <65 would not have been eligible for primary prevention by the criteria of the ACC/AHA or, most probably, by any of the guidelines. There’s too little action when action arguably matters most. The timing of the guidelines is out of sync. However, by adopting age- and sex-specific thresholds, a good portion of this could be rectified.7
The Causal Model of Cardiovascular Events: LDL Matters
The strengths as well as the limitations of this approach are set out in greater detail elsewhere.4 Here, only a few of the principal points will be summarized. With the exception of those with extreme elevations of LDL, the risk model states that risk assessment adequately incorporates the risk resulting from LDL. We dispute this. Atherosclerosis is undoubtedly multifactorial in origin. Nevertheless, retention of apoB particles — in particular, retention of LDL particles — is the fundamental event that leads to the initiation, propagation, and maturation of atherosclerotic disease.3 (Figure 2)
The importance of LDL even when 10-year risk has been accounted for is evident in the Framingham study.8 For those with a non-high-density-lipoprotein cholesterol (non-HDL-C) of >160 mg/dl, at median 15-year follow-up CHD rates were 4.4 percent for those with no exposure to elevated non-HDL-C, 8.1 percent for those with one to 10 years of exposure, and 16.5 percent for those with 11 to 20 years of exposure (P <0.001). Overall, 85 percent of young adults with prolonged hyperlipidemia would not have been recommended for statin therapy at 40 years of age under ACC/AHA guidelines.8 These data demonstrate, simply and unequivocally, that selection of subjects for primary prevention can be improved if moderate hyperlipidemia and its duration are taken into account along with the estimate of risk.
 3. Benefit from LDL-lowering therapy relates to LDL as well as risk. Absolute benefit from LDL-lowering therapy does relate to risk. The Cholesterol Treatment Trialists (CTT) established this.9 But that is not the full story. Although still not widely appreciated, CTT also demonstrated that the benefit of LDL lowering is related to the baseline level of LDL-C. If lowering of LDL-C by 1 mmol/L is associated with a constant (approximately) 20 percent benefit in reduction in clinical events, it follows — as the night does the day — that the higher the baseline LDL-C, the greater the absolute lowering of LDL-C that is possible and, therefore, the greater the absolute benefit that is possible.10 Moreover, the higher the baseline LDL-C, the greater the absolute decrease that a standard dose of a statin will produce.11 We have confirmed this by demonstrating a direct relation between baseline LDL-C and benefit from statin therapy in the studies included in CTT.10 Independently, Paul Durrington and his colleagues also have demonstrated that subjects at lower risk but with higher LDL-C may benefit more from statin therapy than subjects at higher risk but with lower LDL-C.12
3. Benefit from LDL-lowering therapy relates to LDL as well as risk. Absolute benefit from LDL-lowering therapy does relate to risk. The Cholesterol Treatment Trialists (CTT) established this.9 But that is not the full story. Although still not widely appreciated, CTT also demonstrated that the benefit of LDL lowering is related to the baseline level of LDL-C. If lowering of LDL-C by 1 mmol/L is associated with a constant (approximately) 20 percent benefit in reduction in clinical events, it follows — as the night does the day — that the higher the baseline LDL-C, the greater the absolute lowering of LDL-C that is possible and, therefore, the greater the absolute benefit that is possible.10 Moreover, the higher the baseline LDL-C, the greater the absolute decrease that a standard dose of a statin will produce.11 We have confirmed this by demonstrating a direct relation between baseline LDL-C and benefit from statin therapy in the studies included in CTT.10 Independently, Paul Durrington and his colleagues also have demonstrated that subjects at lower risk but with higher LDL-C may benefit more from statin therapy than subjects at higher risk but with lower LDL-C.12
4. The risk of LDL and, therefore, the potential benefit of LDL lowering relates to age. That the risk resulting from LDL varies with age also is not appreciated. A number of prospective observational studies observed that the risk associated with LDL-C or apoB is less in those who are older compared to those who are younger, but the clearest demonstration of this phenomenon comes from the International Study of Infarct Survival (ISIS) study.13 The hazard ratio (HR) for apoB decreased progressively such that, at the eighth decade, it was half what it was at the fourth decade. The greater the attributable risk, the greater the potential benefit. On this basis, treating elevated LDL is even more worthwhile in younger subjects compared to older subjects.
Summary
The guideline process is of inestimable value, but it is imperfect. Guideline recommendations have taken on a larger-than-life authority. The process is declared to be driven by the highest- quality evidence, not mere opinion, and therefore, the recommendations should be the standard of care. However, multiple recent cholesterol guidelines have considered virtually the same evidence and if the process is only evidence-dependent, the recommendations should be the same — or at the least, very similar. They are not.14 The guideline process is demonstrably not replicable and, therefore, the recommendations must be opinion- based as well as evidence-based. Until this is recognized and remedied, or at least acknowledged, the process will continue to fall short of the necessary standard it should achieve.
We believe the present approach to primary prevention would be considerably improved if the risk thresholds were age- and sex-dependent and if more emphasis were placed on the causes of vascular disease and not simply on the calculated risk of a clinical event. In younger individuals, risk should be projected for longer periods than a decade; 15- or 30-year risk15 for these individuals is more practical and will lead to more meaningful choices than lifetime risk.
Primary prevention needs to be reconfigured so more of the younger subjects and fewer of the older subjects are treated. This would be possible using age- and sex-adjusted thresholds of risk.7 Beyond that, more emphasis needs to be placed on earlier identification of those with moderate but sustained elevation of LDL-C. The evidence from epidemiological studies and randomized controlled trials (RCTs) supports greater emphasis on LDL as a marker of risk and treatment objectives than the guidelines acknowledge.10 Accordingly, accurately measuring the atherogenic potential of LDL is critical. Just as the conventional models to estimate risk have been shown to have important limitations, so have the conventional statistical methods to assess the relative importance of highly correlated markers of LDL such as LDL-C, non-HDL-C and apoB.16 Newer approaches, such as discordance analysis, overcome these limitations and demonstrate that apoB is superior to LDL-C and non-HDL-C as a marker of cardiovascular risk.17,18
In summary, much has been achieved but much more can be achieved if we reconfigure primary prevention to place greater emphasis on LDL as the primary cause of atherosclerosis, which is the primary cause of clinical vascular events. If we prevent the disease, we will not have to worry about the events.
Disclosure statement: Dr. Sniderman received speaker honorarium from Cleveland HeartLab. Dr. Willard has no disclosures to report.
References are listed on page 37 of the PDF.






.jpg)
.png)












