The intent of this article is to review the over-the-counter (OTC) products and dietary supplements that have proven effective on cholesterol levels. There is little direct evidence of how these supplements affect cardiovascular outcomes. Additionally, the dosage forms, recommended daily dosage, and content of these products often vary among manufacturers.
OTC medications differ from dietary supplements in terms of their U.S. Food and Drug Administration (FDA) regulatory requirements. The FDA review of all available OTC drugs is completed by the Center for Drug Evaluation’s Office of Drug Evaluation IV. OTC medications are developed under the OTC Monograph Process or through the New Drug Application (NDA) Process. Any company or sponsor seeking to market or produce their product for OTC sale applies to the Division of Nonprescription Drug Products (DNDP) in the Office of Drug Evaluation IV. The DNDP reviews consumer studies and post-marketing safety data, as well as original efficacy data, drug development, labeling, and any regulatory issues.
The DNDP also is responsible for the development of OTC drug monographs. Any other supplementary information or reviews needed may be acquired from additional disciplines or divisions within the Office of New Drugs.1
Many products are considered dietary supplements and, unlike OTC medications, the FDA does not regulate them. They also aren’t required to go through any type of drug approval process. Any company or sponsor, prior to marketing a dietary supplement, is required to confirm that their product — whether manufactured or distributed — is safe, any claims made about the product are not false or misleading, and the product complies with the Federal Food, Drug and Cosmetic Act and FDA regulations in all other respects.2
The focus of this review will be limited to some of the available OTC products and dietary supplements that have proven beneficial in lowering serum cholesterol levels. The following products may be considered as an adjunct or, in some cases, a supplement to conventional pharmacotherapy.
Artichoke Leaf Extract
Artichoke leaf extract (ALE) has key active components, including caffeoylquinic acids, flavonoids, and bitters that have been studied and proposed to have both hypocholesterolemic and antioxidant properties. The proposed mechanism of action is similar to statins. The mechanism of action is suggestive of a reduction in intrinsic cholesterol synthesis through HMG CoA reductase inhibition, LDL-C oxidation inhibition, and increased elimination of cholesterol through bile secretions.3 A study conducted in Germany in the 1990s4 consisted of 143 patients with LDL-C levels greater than 280mg/dL who were randomized into two groups taking either 1,800 mg of dr y artichoke extract daily or a placebo. After a six- week treatment period, they found that patients taking artichoke extract had significant reduction in total cholesterol (18.5 percent) compared to the placebo group (8.6 percent) and LDL-C reduction in patients taking artichoke extract (22.9 percent) compared to the placebo group (6.3 percent). Other recent studies have had conflicting data and do not reproduce results. There is weak supporting information to make a recommendation for use or against use of artichoke leaf extract for the use of hyperlipidemia.
Coenzyme Q10
Coenzyme Q10, also known as CoQ10 and ubiquinone, is a naturally synthesized compound found in the body, concentrated in mitochondria. CoQ10 synthesis is inhibited by statins. Its proposed mechanism includes antioxidant properties on LDL-C as well as energy generation as a player in the electron transport chain within the mitochondria. It is often taken in conjunction with statins to reduce CoQ10 deficiency and decrease risk of myalgia.5,6 Few studies have been conducted with CoQ10 as monotherapy for cholesterol reduction. A 2003 study5 compared the effects of CoQ10 120 mg daily vs. vitamin B in 144 subjects post-MI and found no difference in reductions in total cholesterol or LDL-C. In addition, the CoQ10 treatment group had a statistically significant increase in HDL-C levels.
Another study7 examined the effects of adding CoQ10 100 mg daily or placebo to atorvastatin 10 mg daily — and there are no differences in total cholesterol, LDL-C, HDL-C, or TGs after 12 weeks. There was a statistically significant difference in mean level of plasma total CoQ10 with the CoQ10 treatment group (+127 percent) compared to 42-percent reduction in the placebo group.
There have been several additional studies8 that have tried to demonstrate supplementation effects of CoQ10 but have been unsubstantial due to insufficient doses of CoQ10, short treatment periods, as well as a small number of study participants. Although there are disputable results of previous studies for monotherapy of CoQ10, there is a role for CoQ10 supplementation to enable better tolerability of statin therapy.
Fiber
Fiber can be classified as insoluble and soluble. The proposed mechanism of soluble fiber for reduction in LDL-C and total cholesterol is thought to be through a reduced glycemic response that produces reduced insulin stimulation of hepatic cholesterol synthesis and prevents the resorption of bile salts from the small intestine, resulting in increased excretion of bile salts. Soluble fibers include psyllium, oats, flaxseed, and barley.9,10
Fenugreek is a spice, naturally found in seed form, which is used as a source of soluble fiber supplementation. There are a number of studies11,12 demonstrating the effects of fenugreek, but some have shown total cholesterol reduction of 14 percent, LDL-C reduction of 15 percent, TG reduction of 15 percent, and HDL-C increase of 10 percent.
A 1999 meta-analysis13 that included 67 clinical trials concluded that diets with a high intake of soluble fiber were associated with a 60 to 70 percent reduction in total cholesterol, as well as a reduction in LDL-C levels, though no percentage was provided for the LDL-C reduction. Practical application of these results is limited because of the amount of soluble fiber ingested per patient.
The analysis suggested that the daily intake of 3 gram of soluble fiber would decrease total cholesterol approximately 2 percent. The U.S. Department of Agriculture recommends a daily intake of approximately 25 grams to 35 grams of soluble fiber.
In a recent review of dietary supplements,10 a pooled analysis of 10 cohort studies observed that each 10 gram per day increase in dietary fiber correlated with a 12 percent reduction in the risk of coronary events and a 19 percent reduction in the risk of coronary deaths. An additional meta-analysis found a small but significant 7-percent reduction in LDL-C with the daily ingestion of 2 grams to 10 grams of soluble fiber. While a range of LDL-C and total cholesterol reductions and CV morbidity/mortality response has been reported, it is recommended by the U.S. Department of Health and Human Sciences that patients should have a daily intake of at least 5 grams to 10 grams of soluble fiber either incorporated into foods or taken as an additional supplement.
Flaxseed
Flaxseed has been identified as a plant-source alternative to omega-3 polyunsaturated fatty acids (PUFAs), better known as fish oil. Flaxseed oil is largely composed of acid alpha-linolenic acid (ALA), which can be converted to docosahexanoic acid (DHA) and eicosapentanoic acid (EPA). Flaxseed oil’s mechanism of cholesterol reduction is not well understood but may include the inhibition of acyl coenzyme A (CoA)-1,2 diacylglycerol acyltransferase (DGAT), enhanced plasma lipoprotein lipase activity, decreased lipogenesis in the liver, and increased beta-oxidation activity in mitochondria and peroxisomes in the liver.10 In a study of 62 patients published by the Journal of the American College of Nutrition,14 they enrolled patients with LDL-C levels between 130mg/dL and 200mg/dL that received either 40 grams of flaxseed-containing baked products daily or matching wheat bran products for 10 weeks in addition to a low-fat, low- cholesterol diet. There was a significant decrease (13 percent) in LDL-C levels of the flaxseed treatment group at five weeks but not significant (7 percent) at 10 weeks. They also found that HDL-C levels were significantly reduced at both five weeks (16 percent) and 10 weeks (9 percent). There are inconsistent results from other similar studies15 that raise questions about the supplement’s ability to lower serum cholesterol. Flaxseed is considered a source of soluble fiber and a supplement with at least 5 grams to 10 grams daily is recommended for risk reduction in coronar y events and modest reductions in cholesterol levels.
Fish Oil/Omega-3 Fatty Acids
Fish oil, or omega-3 fatty acid, has been studied for its triglyceride-reduction ability. Omega-3 fatty acids are largely composed of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). There are several prescription products and multiple OTC supplements available.
The mechanism of action is believed to include the inhibition of acyl coenzyme A (CoA)-1,2 diacylglycerol acyltransferase (DGAT), enhanced plasma lipoprotein lipase activity, decreased lipogenesis in the liver, and increased beta-oxidation activity in mitochondria and peroxisomes in the liver.16 It has also been hypothesized to have antiplatelet and anti-inflammator y properties.17 There have been many studies demonstrating fish oil’s effect on cholesterol levels. A review of 65 studies was published in the American Journal of Clinical Nutrition,18 concluding that approximately 4 grams of omega-3 fatty acids results in triglyceride reduction of 25 to 30 percent, HDL-C increase of 1 to 3 percent, no change in total cholesterol levels, and an LDL-C increase of 5 to 10 percent.
There is a wide variety of quality and EPA/DHA content between OTC fish oil supplements. Individual patients should have a clear indication for intended use and expectations when selecting their product. Omega-3 fatty acid supplementation is generally recommended as a treatment option for the subset of patients with hypertriglyceridemia, as results have shown a maximum benefit in triglyceride reduction. In patients with mixed dyslipidemia, omega-3 fatty acids may be used in addition to other therapy or supplements that have superior effects of other lipid panel values, such as total cholesterol, HDL-C, and LDL-C.
Garlic
Garlic has often been considered an herbal treatment for high blood pressure, but also has been studied for its cholesterol reduction. It is believed to reduce cholesterol by inhibiting enzymes involved in lipid synthesis, increasing antioxidant properties within the body, decreasing platelet aggregation, and preventing lipid peroxidation of LDL and er ythrocytes.10,19
In 2010, the U.S. Department of Health and Human Services released a report20 stating garlic produced small, short-term (approximately three months) reductions in both LDL-C and total cholesterol. A study21 of 192 patients with LDL-C levels ranging from 130mg/dL to 190mg/dL. Participants were assigned to one of four possible treatment groups receiving: raw garlic, a powdered garlic supplement, an aged garlic extract supplement, or a placebo. They concluded that none of the garlic supplements had any significant effect on LDL-C, HDL-C, total cholesterol, or triglycerides after six months. There is concern regarding the bioavailability of garlic, the potency of its active ingredient, and the variety of dosage forms available. Based on the lack of any significant evidence, it appears that garlic has little to no effect on cholesterol levels and should not be recommended for use.
Ginseng
Ginseng is available in a variety of dosage forms, depending on the ginseng plant used. A majority of clinical studies involve the Panax species; this species contains ginsenosides or glycosides, which are thought to be the main active cholesterol-lowering component in ginseng. Studies have shown more than 30 ginsenosides exist in ginseng, along with fatty acids, peptides, and polysaccharides. It is believed to reduce cholesterol by inhibiting carbohydrate absorption in the intestines and results in proliferation of peroxisome-activated receptors. Buettner, et al22 reviewed six clinical trials of ginseng’s effects on cholesterol levels and found the results were inconsistent, with total cholesterol levels ranging from a 29-percent reduction to a 7-percent increase, LDL-C levels ranging from a 45-percent reduction to an 11-percent increase, and triglyceride levels ranging from a 24-percent reduction to a 10.5-percent increase. The authors concluded that there were insufficient well-designed, randomized, controlled studies to make any recommendations for the use of ginseng in cholesterol reduction.
Guggul
Guggul is an extract collected from mukul myrrh tree (Commiphora mukul) resin. It has been postulated that E-guggulsterone and Z-guggulsterone are present within the extract. Research has shown that guggulsterones have inhibitive activity against the bile acid receptor and farnesoid X receptor (FXR) involved with cholesterol metabolism and bile acid regulation.10
Szapary, et al23 demonstrated that standard- and high-dose guggul resulted in a 4- and 5-percent increase in LDL-C levels, respectively, with no significant changes in total cholesterol, HDL-C, or TG levels after eight weeks. It appears that guggul has no benefit in lowering cholesterol and should not be recommended for use.
Availability
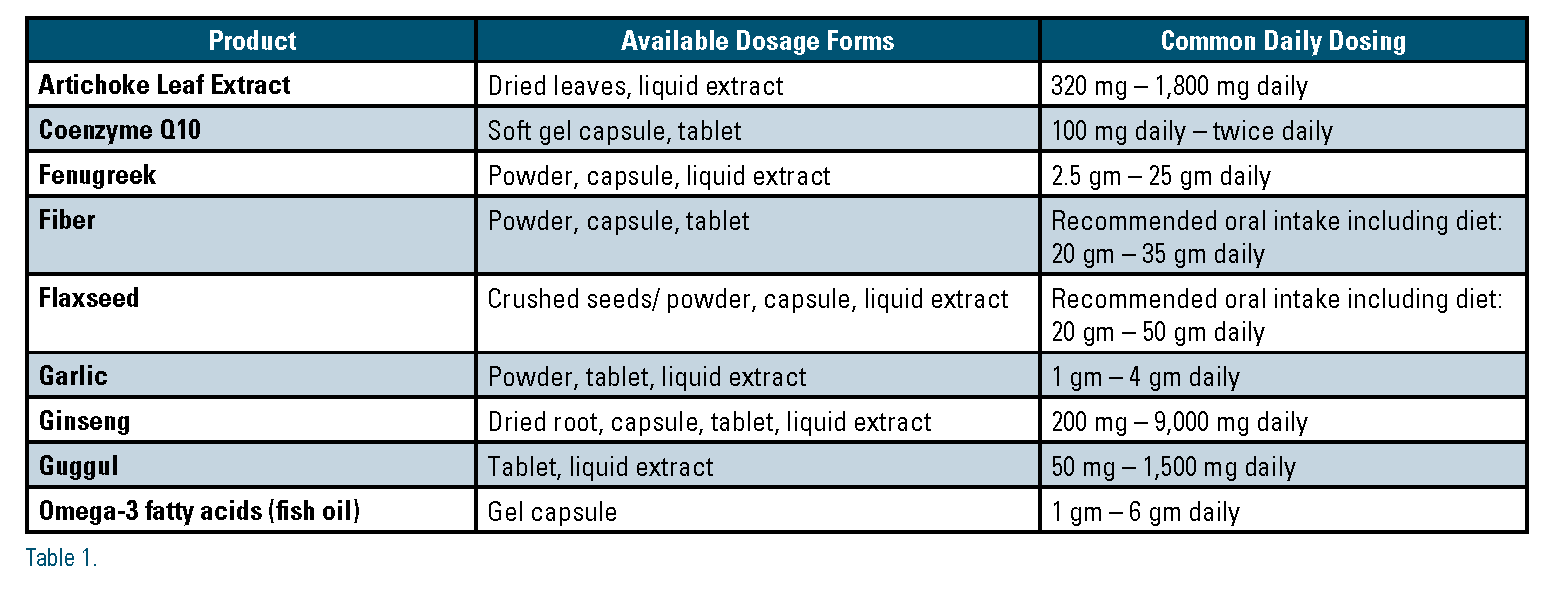
All of the dietary supplements discussed above can be found in various dosage formulations, produced from numerous manufacturers, and available from quite a few drug stores or herbal/dietary market stores. Using the database Natural Medicines,24 Table 1 represents some of the various dosage forms available and the common daily-dosing regimens.
Conclusion
There are a number of OTC dietar y supplements studied for their cholesterol- lowering effects. Artichoke leaf extract, fenugreek, and ginseng supplements have inadequate data supporting efficacy. Both garlic and guggul supplements have been shown to have no beneficial effect on cholesterol-lowering. Coenzyme Q10, fiber, flaxseed, omega-3 fatty acids, and red yeast rice products all have data that support their use as dietar y supplements. Consumers should thoroughly review the available ingredients and contents and inform their healthcare provider before using any of these supplements.
Disclosure statement: Dr. Kellick has no disclosures to report. Dr. Conway has no disclosures to report.
References are listed on page 36 of the PDF.





.jpg)
.png)













Comments
OTC
OTC products are regulated by the FDA: most if not all of the above mentions supplements are food supplements and not OTC products