Mr. P is a 63-year-old male with a known history of coronary artery disease (CAD) who developed chest pressure and tightness while riding his motorcycle in the White Mountains in Northern Arizona. Since there wasn’t much traffic, he continued to ride but soon began to feel clammy and nauseated. Fortunately, he was able to get to the next town and went to the local hospital, where he underwent cardiac evaluation. He was found to have non-ST-segment elevation-acute coronary syndrome. Cardiac catheterization revealed a high-grade stenosis in the proximal left anterior descending (LAD) artery that was angioplastied and stented. He had residual disease with a known chronic total occlusion (CTO) in his right coronary artery (RCA) and his primary Cardiologist agreed that medical management is appropriate.
Mr. P has a history of CAD with a 2009 myocardial infarction (MI) for which he underwent staged percutaneous coronary interventions (PCI) with stenting of his LAD followed by stenting of an obtuse marginal branch. He developed recurrent symptoms 5 months later and underwent PCI to a de novo lesion in his distal LAD. In addition to his CAD, Mr. P has a history of asthma, deep-vein thrombosis and pulmonary embolus (treated with warfarin).
Risk factors for the progression of his arteriosclerotic cardiovascular disease (ASCVD) include type II diabetes, hypertension, obesity, metabolic syndrome with dyslipidemia, and human immunodeficiency virus (HIV).
The atorvastatin was increased from 20mg to 40mg. Although he was taking atorvastatin, he reported an allergy to statins and previously had been on pravastatin and trialed rosuvastatin. Other medications included valsartan 80mg, clopidogrel, ipratropium inhaler, and warfarin. He is also taking ritonovir, (protease inhibitor) abacavir/ lamivudine (nucleoside/nucleotide reverse transcriptase inhibitors [NNRTIs]) and darunavir with food (protease inhibitor).
Because of multiple comorbidities, he was referred to the lipid center.
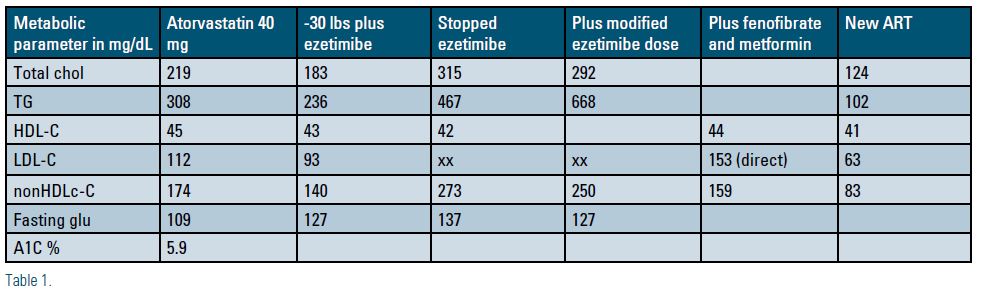
Lab findings on maximally tolerated statin revealed a total cholesterol of 219 mg/dL, low-density lipoprotein cholesterol (LDL-C) 112 mg/dL, non-high-density lipoprotein cholesterol (non-HDL-C) 174mg/dL, high-density lipoprotein cholesterol (HDL-C) 45 mg/dL, triglyceride (TG) 308mg/dL, glucose 109 mg/dL and hemoglobin A1c (Hgb A1c) 5.9%. Ezetimibe was added to his regimen and when he returned to the lipid clinic he had achieved a 30 lb weight loss. Labs now revealed total cholesterol (TC) 183mg/dL, LDL-C 93 mg/dL, non-HDL-C 140mg/dL, HDL-C 43mg/dL, TG 236mg/dL, glucose 127mg/dL, weight 255.4 pounds.
On his return to the lipid clinic in May 2016, his lab now revealed glucose 137mg/dL, TC 315mg/dL, TG 467 mg/dL, non-HDL-C 273mg/dL and HDL 42 mg/ dL. He had stopped his ezetimibe because he felt it was worsening his asthma and had developed leg pain. He agreed to a modified dosing regimen of ezetimibe.
A repeat lipid profile demonstrated: TC 292 mg/dL, TG 668mg/dL, non-HDL-C 250 mg/dL, glucose 127 mg/dL prompting the prescription of low-dose fenofibrate and metformin was recommended and follow-up labs revealed TC 203 mg/dL, direct LDL-C 153 mg/dL, non-HDL-C 159mg/dL, TG 216 mg/dL and HDL-C 44 mg/dL.
At this point, Mr. P was on maximally tolerated statin and ezetimibe and low dose fenofibrate. Based upon the complexity of the condition, and with the patient’s consent, we discussed his case with colleagues from the NLA with known expertise in managing patients with HIV. The protease inhibitors were identified as the culprit and changes to the patient’s antiretroviral therapy were recommended. As a result of this collaboration and subsequent recommendations, the immunologist agreed to change his ART1 resulting in the following lipid profile: TC 124 mg/dL, LDL-c 63 mg/dL, non-HDL-C 83 mg/dL, HDL 41 mg/dL and TG 102 mg/dL.
HIV-infected patients are at increased risk for development and progression of ASCVD with increased incidence of MI and cardiovascular disease (CVD) mortality.2,3 According to the National Lipid Association (NLA) HIV infection should be considered equivalent to one additional ASCVD risk factor.4,5 However, not only does HIV infection increase ASCVD risk, HIV treatment with ART can worsen a patient’s cardiometabolic risk profile. ART has been associated with adverse effects on insulin resistance, hyperglycemia and lipid abnormalities.5,6 Further complicating management, many drug-drug interactions have been noted between ART and lipid-lowering therapies, because protease inhibitors, NNRTIs and some statins are metabolized by the same CYP450 pathways.7 Given Mr. P’s history of ASCVD, high-intensity statin is indicated but must be used with caution because of interactions with his ART.4
Mr. P reached his LDL-C and non-HDL-C goals and remains in stable condition with no recurrent events or ischemic symptoms. This case study illustrates how a seemingly straightforward case can represent a complex management dilemma requiring collaboration of multiple specialists to recognize and define each facet of these complexities and sometimes requires changes in therapy in deference to another’s expertise. Fortunately, Mr. P had access to a healthcare team – consisting of a PCP/immunology specialist, a diabetes specialist, a dietitian, a cardiologist and a lipid specialist – that, in collaboration with experts in HIV management, partnered with him to optimize his disease management.
I would like to thank: Dr. Santiago Ramirez, Interventional Cardiology, Southern Arizona Heart and Vascular, Tucson, Arizona, Dr. Kevin Carmichael, PCP/Immunology specialist, El Rio Health Center, Tucson, Arizona, Dr. Karen Aspry, director, Lipid and Prevention Program, Lifespan Cardiovascular Institute, Brown University and Dr. Judith Aberg, New York University School of Medicine for contributions to this case study.
Disclosure Statement: Ms. Ciffone was on the speakers bureau for Amgen, Sanofi, Regeneron and Amarin.
References can be found here.





.jpg)
.png)