Lipid lowering therapy is a cornerstone of cardiovascular risk reduction. However, withholding or stopping lipid lowering therapy may be worth consideration in some individuals. These include elderly patients with comorbidities limiting life expectancy, individuals with a coronary artery calcium score of 0 (CAC =0), patients with end stage renal disease (ESRD), and pregnant and lactating women. This review will discuss these scenarios.
Primary Prevention in Elderly Patients with Significant Comorbidities and Limited Life Expectancy
Recommendations for primary prevention of atherosclerotic cardiovascular disease (ASCVD) in adults > 75 years are limited. The 2018 multi-society cholesterol guidelines excluded patients in this age group.1 Decisions in these patients are complicated by factors such as frailty, polypharmacy, and cognitive impairment, as well as a paucity of data in this population.2,3
The Copenhagen general population study enrolled 90,000 individuals aged 20-100 years. Adults aged 80-100 years had the highest absolute risk of a myocardial infarction (MI), the risk increasing with higher LDL levels. This group also had the lowest calculated number needed to treat (NNT, 80) to prevent an MI in 5 years.4 In contrast, the PROspective Study of Pravastatin in the Elderly at Risk (PROSPER) trial found no major adverse cardiac events (MACE) benefit with pravastatin use for primary prevention in adults ages 70-82 years.5
The PRagmatic EValuation of evENTs and Benefits of Lipid lowering in oldEr adults (PREVENTABLE, NCT04262206) will assess the effects of statins on dementia, disability, cardiovascular death, and cognitive disability in adults >75 years. The Statins in Reducing Events in the Elderly (STAREE, NCT04536870) trial will compare the effects of atorvastatin vs placebo on disability, frailty, and major CV events. Statins In The Elderly (SITE, NCT02547883) is evaluating the effect of withdrawing statins on all-cause mortality and incremental cost per quality-of-life years gained in adults ≥ 75 years.6 While these findings are awaited, shared decision making of risks versus benefits evaluating competing comorbidities, atherosclerotic disease burden, and considering the impact of a cardiovascular event on quality of life may aid decision-making in this population.
The Power of Zero
Many studies have demonstrated a lower risk of cardiovascular outcomes and all-cause mortality among individuals with CAC = 0 as compared with CAC > 0, even after adjusting for traditional risk factors.7,8 Patients with a CAC = 0 had a 10-year risk below the threshold for statin initiation (4.5%) even with a calculated 10-year ASCVD risk in the 7.5-20% range, and with risk enhancers9,10 like hsCRP > 2 mg/dL.
Withholding statin therapy in individuals with CAC = 0 has been evaluated in two retrospective studies. Out of 950 subjects from the Multiethnic Study of Atherosclerosis (MESA) with a high sensitivity CRP of > 2 mg/dL, the 5-year NNT for statin use was 124 in these subjects9 versus 19 in those with CAC > 0. In a Walter Reed study11 with 10-year follow up, statin use was not associated with a lower risk of MACE in individuals with CAC = 0. The 2018 Multisociety guideline on the Management of Blood Cholesterol1 suggests that adults 40-75 years without diabetes, cigarette smoking, or strong family history of premature ASCVD can delay or withhold statin initiation with a CAC =0 (de-risking).
Certain considerations, however, should refine the choice to withhold statins in patients having a CAC=0. The data on the long-term prognostic significance of CAC = 0 in young adults are emerging.12 In a cohort study, 25% of patients with CAC = 0 developed CAC in 5 years.13 This duration was shorter in patients with a high burden of risk factors like diabetes suggesting serial testing at 3-5 years may be needed in these individuals.14–16 Lastly, patients with heterozygous FH, even with a CAC = 0, are conventionally treated with at least a statin.17 For many patients with uncertainty in individual risk, a CAC = 0 may help with shared decision making around statin initiation. The approach for these patients could include a focus on lifestyle management with periodic re-estimation of risk.
End Stage Renal Disease (ESRD)
Four randomized controlled trials (RCT) evaluated the effect of statins in patients with ESRD undergoing hemodialysis (HD). The 4D study found no statistically significant effects on cardiovascular death, non-fatal MI, and non-fatal stroke with atorvastatin 20 mg/day in diabetic patients with and without ASCVD, on HD.18 Similar results were noted in the AURORA (A Study to Evaluate the Use of Rosuvastatin in Subjects on Regular Hemodialysis: An Assessment of Survival and Cardiovascular Events) with rosuvastatin 10 mg/day.19 SHARP (Study of Heart and Renal Protection) evaluated a combination of simvastatin and ezetimibe in a primary prevention cohort with CKD, with and without HD, finding a 27% benefit in major vascular events compared with placebo. In subgroup analysis, the benefit was seen in the non – HD cohort but not the HD cohort. However, the trial was not powered for this analysis.20
Whether the lack of benefit in these trials was due to a lower dose of statins being used or competing risks of death in this population is not fully understood. The Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend against the routine initiation of a statin in all comers with ESRD but recommend continuation if already receiving a statin.21
Pregnancy and Lactation
Statins have traditionally been contraindicated when pregnancy is planned and during pregnancy due to concerns of teratogenicity and unfavorable effects on metabolic pathways that regulate morphogenesis demonstrated in pre-clinical animal models.22,23 Women are advised against statin therapy until the cessation of lactation due to the potential detrimental effects on cholesterol biosynthesis in the neonate. Most statins can be found in breast milk, however, specific information on the type of statin and how much can cross into breast milk is limited.
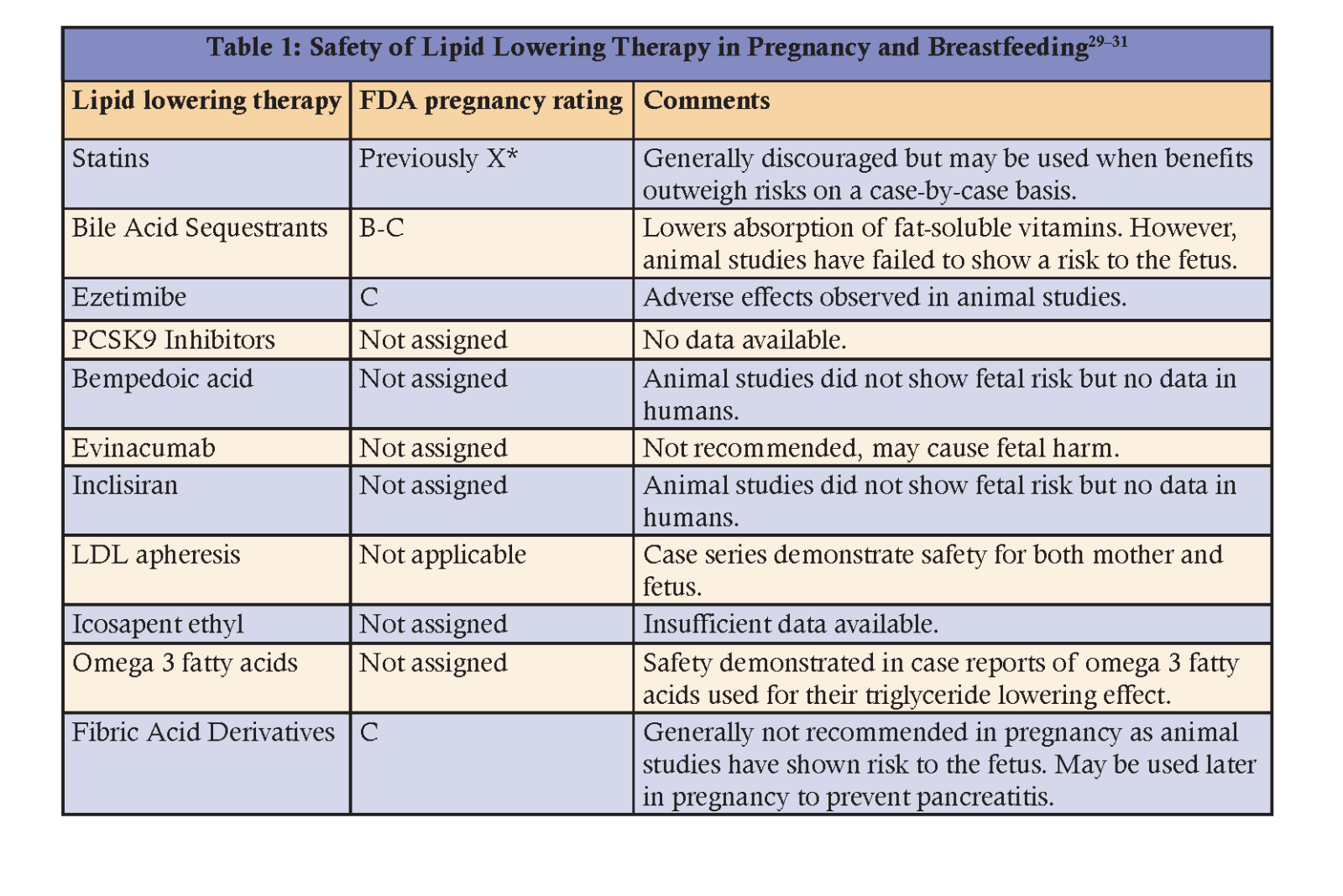
More recent systematic reviews and meta-analyses did not demonstrate clear associations between statin use and teratogenicity and seem to suggest that statins are, “probably not teratogenic”.24–26 In 2021 the Food and Drug Administration removed the strongest warnings against statin use during pregnancy.27 However, barring certain high-risk patients like homozygous FH or prior ASCVD events, current guidelines still recommend holding statins during pregnancy and lactation.1,28 Table 1 describes the common considerations for lipid lowering medications in pregnancy and lactation.
Conclusion
The benefits of lipid lowering therapy in ASCVD prevention have been well described and widely adopted. However, the benefits from therapy are not uniform across patient subgroups. This review aims to empower clinicians to have a nuanced risk-benefit discussion based on each individual patient’s clinical profile.
Dr. Satish has no financial relationships to disclose. Dr. D’Souza has no financial relationships to disclose. Dr. Agarwala has no financial relationships to disclose.
References
- Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Jun 18;139(25):e1082–143.
- Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA. 2004 Apr 21;291(15):1864–70.
- Montgomery S, Miedema MD, Dodson JA. Aspirin and statin therapy for primary prevention of cardiovascular disease in older adults. Heart. 2022 Jul 1;108(14):1090–7.
- Mortensen MB, Nordestgaard BG. Elevated LDL cholesterol and increased risk of myocardial infarction and atherosclerotic cardiovascular disease in individuals aged 70–100 years: a contemporary primary prevention cohort. The Lancet. 2020 Nov 21;396(10263):1644–52.
- Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. The Lancet. 2002 Nov 23;360(9346):1623–30.
- Bonnet F, Bénard A, Poulizac P, Afonso M, Maillard A, Salvo F, et al. Discontinuing statins or not in the elderly? Study protocol for a randomized controlled trial. Trials. 2020 Apr 19;21:342.
- Nasir K, Cainzos-Achirica M. Role of coronary artery calcium score in the primary prevention of cardiovascular disease. BMJ. 2021 May 4;n776.
- Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffman U, Cury RC, et al. Diagnostic and Prognostic Value of Absence of Coronary Artery Calcification. JACC: Cardiovascular Imaging. 2009 Jun;2(6):675–88.
- Blaha MJ, Budoff MJ, DeFilippis AP, Blankstein R, Rivera JJ, Agatston A, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. The Lancet. 2011 Aug 20;378(9792):684–92.
- Nasir K, Bittencourt MS, Blaha MJ, Blankstein R, Agatson AS, Rivera JJ, et al. Implications of Coronary Artery Calcium Testing Among Statin Candidates According to American College of Cardiology/American Heart Association Cholesterol Management Guidelines. Journal of the American College of Cardiology. 2015 Oct 13;66(15):1657–68.
- Mitchell JD, Fergestrom N, Gage BF, Paisley R, Moon P, Novak E, et al. Impact of Statins on Cardiovascular Outcomes Following Coronary Artery Calcium Scoring. Journal of the American College of Cardiology. 2018 Dec 25;72(25):3233–42.
- Miedema MD, Dardari ZA, Nasir K, Blankstein R, Knickelbine T, Oberembt S, et al. Association of Coronary Artery Calcium With Long-term, Cause-Specific Mortality Among Young Adults. JAMA Network Open. 2019 Jul 19;2(7):e197440.
- Min JK, Lin FY, Gidseg DS, Weinsaft JW, Berman DS, Shaw LJ, et al. Determinants of Coronary Calcium Conversion Among Patients With a Normal Coronary Calcium Scan. Journal of the American College of Cardiology. 2010 Mar 16;55(11):1110–7.
- Lee JH, Han D, ó Hartaigh B, Rizvi A, Gransar H, Park HB, et al. Warranty Period of Zero Coronary Artery Calcium Score for Predicting All-Cause Mortality According to Cardiac Risk Burden in Asymptomatic Korean Adults. Circ J. 2016;80(11):2356–61.
- Valenti V, ó Hartaigh B, Heo R, Cho I, Schulman -Marcus Joshua, Gransar H, et al. A 15-Year Warranty Period for Asymptomatic Individuals Without Coronary Artery Calcium. JACC: Cardiovascular Imaging. 2015 Aug;8(8):900–9.
- Dzaye O, Dardari ZA, Cainzos -Achirica Miguel, Blankstein R, Agatston AS, Duebgen M, et al. Warranty Period of a Calcium Score of Zero. JACC: Cardiovascular Imaging. 2021 May;14(5):990–1002.
- Mszar R, Nasir K, Santos RD. Coronary Artery Calcification in Familial Hypercholesterolemia. Circulation. 2020 Oct 13;142(15):1405–7.
- Wanner C, Krane V, März W, Olschewski M, Mann JFE, Ruf G, et al. Atorvastatin in Patients with Type 2 Diabetes Mellitus Undergoing Hemodialysis. N Engl J Med. 2005 Jul 21;353(3):238–48.
- Fellström BC, Jardine AG, Schmieder RE, Holdaas H, Bannister K, Beutler J, et al. Rosuvastatin and Cardiovascular Events in Patients Undergoing Hemodialysis. N Engl J Med. 2009 Apr 2;360(14):1395–407.
- Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet. 2011 Jun 25;377(9784):2181–92.
- Wanner C, Tonelli M, Kidney Disease: Improving Global Outcomes Lipid Guideline Development Work Group Members. KDIGO Clinical Practice Guideline for Lipid Management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int. 2014 Jun;85(6):1303–9.
- MacDonald JS, Gerson RJ, Kornbrust DJ, Kloss MW, Prahalada S, Berry PH, et al. Preclinical evaluation of lovastatin. Am J Cardiol. 1988 Nov 11;62(15):16J-27J.
- Pollack PS, Shields KE, Burnett DM, Osborne MJ, Cunningham ML, Stepanavage ME. Pregnancy outcomes after maternal exposure to simvastatin and lovastatin. Birth Defects Res A Clin Mol Teratol. 2005 Nov;73(11):888–96.
- Karalis DG, Hill AN, Clifton S, Wild RA. The risks of statin use in pregnancy: A systematic review. J Clin Lipidol. 2016 Oct;10(5):1081–90.
- Kusters DM, Hassani Lahsinoui H, van de Post JAM, Wiegman A, Wijburg FA, Kastelein JJP, et al. Statin use during pregnancy: a systematic review and meta-analysis. Expert Rev Cardiovasc Ther. 2012 Mar;10(3):363–78.
- Zarek J, Koren G. The fetal safety of statins: a systematic review and meta-analysis. J Obstet Gynaecol Can. 2014 Jun;36(6):506–9.
- Commissioner O of the. Statins: Drug Safety Communication - FDA Requests Removal of Strongest Warning Against Using Cholesterol-lowering Statins During Pregnancy. FDA [Internet]. 2021 Jul 20 [cited 2022 Nov 6]; Available from: https://www.fda.gov/safety/medical-product-safety-information/statins-drug-safety-communication-fda-requests-removal-strongest-warning-against-using-cholesterol
- Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019 Nov 1;290:140–205.
- Grant JK, Snow S, Kelsey M, Rymer J, Schaffer AE, Patel MR, et al. Lipid-Lowering Therapy in Women of Childbearing Age: a Review and Stepwise Clinical Approach. Curr Cardiol Rep. 2022 Oct;24(10):1373–85.
- Poornima IG, Pulipati VP, Brinton EA, Wild RA. Update on Statin Use in Pregnancy. Am J Med. 2023 Jan;136(1):12–4.
- Kaur G, Gulati M. Considerations for treatment of lipid disorders during pregnancy and breastfeeding. Progress in Cardiovascular Diseases. 2022 Nov 1;75:33–9.
Article By:
PGY-6 Cardiology fellow
Houston Methodist DeBakey Heart and Vascular Center
Houston, TX
Clinical Lipid Specialist
St. Luke’s Idaho Endocrinology
Boise, ID
Clinical Assistant Professor
Texas A&M University College of Medicine
Center for Cardiovascular Disease Prevention
Cardiovascular Division
Baylor Scott and White Health Heart Hospital Baylor Plano
Plano, TX





.jpg)
.png)










