As an Internist who specialized in adult medicine, I had not seen many pediatric patients since my days in medical school. Now, however, as a Clinical Lipidologist, I have had the opportunity on a few occasions to evaluate a child or young adolescent with markedly elevated LDL cholesterol referred by pediatric and family medicine colleagues. Despite the increase prevalence of childhood obesity, diabetes, and dyslipidemia, these problems are still best treated by lifestyle changes of healthier diet, more exercise, and in many cases do not require pharmacologic intervention.
This review focuses on the screening and diagnosis of heterozygous familial hypercholesterolemia (HeFH,) including appropriate cardiovascular risk assessment with current treatment recommendations. Guidelines reviewed include the 2008 policy statement by the American Academy of Pediatrics (AAP - Lipid Screening and Cardiovascular Health in Children, the 2008 National Institute for Health and Clinical Excellence (NICE) Clinical Guidelines - Identification & Management of Familial Hypercholesterolemia, the June 2011 National Lipid Association (NLA) Expert Panel on FH - Familial Hypercholesterolemia: Screening, Diagnosis, and Management of Pediatric and Adult Patients, and the NHLBI Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reductions in Children and Adolescents: Summary Report.1,2,3
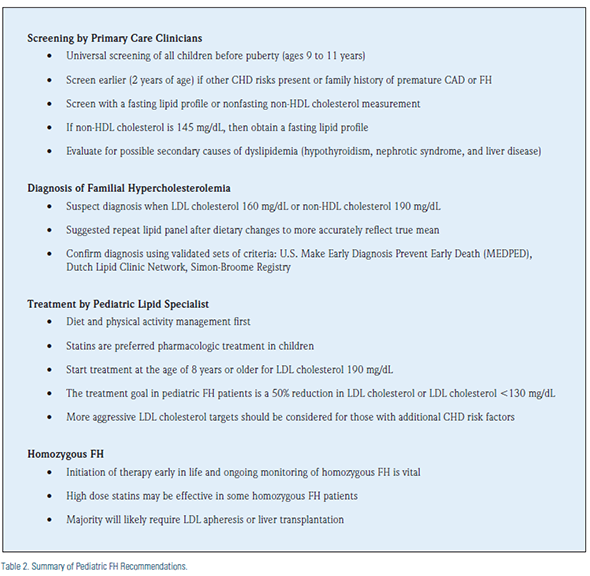
Screening: Universal lipid screening for all children is recommended between ages 9 to 11.1,2,3 Previous guidelines had recommended only screening for cholesterol if there was a clear family history of FH or premature CHD.
This recommendation of selective screening based on family history, however, misses about 30-60% of children and adolescents with HeFH, with the greatest risk for premature CHD. The age of 9-11 for routine, universal screening was selected because cholesterol values later, during the age of puberty (especially ages 14-16), tend to be lower than pre-pubescent age, are more variable (less reproducible), and are less sensitive to detect patients at higher cardiovascular risk from FH.
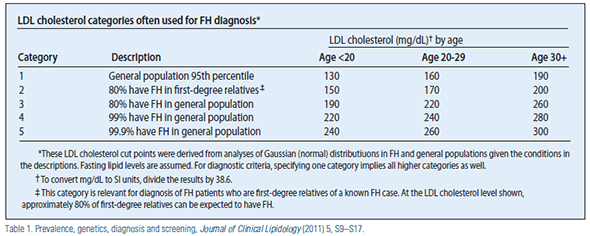
Initial screening is recommended with either a fasting lipid panel or nonfasting non-HDL cholesterol (total cholesterol minus HDL cholesterol) If the non- HDL cholesterol is 145 mg/dL, then a traditional lipid panel is advised. Results are considered elevated when they are over the 95th percentile (LDL cholesterol greater than 130 and total cholesterol greater than 200–see Table 1). Screening should be performed earlier (after two years of age) in the presence of other major CHD risk factors, or if there is a high index of suspicion for FH based upon positive family history of FH or premature coronary heart disease (CHD). In addition to cholesterol testing, evaluation for secondary causes of dyslipidemia should include a focused history, physical exam, and select testing for diseases like hypothyroidism, nephrotic syndrome, and liver disease.
Diagnosis of FH: For children, adolescents, and young adults (< 20 years) FH may be suspected when the LDL cholesterol is 160 mg/dL or non-HDL cholesterol is 190 mg/dL. A follow-up lipid profile should be obtained after appropriate dietary changes, especially in borderline cases, to more accurately assess the mean result. Formal clinical diagnosis of FH can be made by applying any one of several validated sets of criteria [U.S. Make Early Diagnosis Prevent Early Death (MEDPED), Dutch Lipid Clinic Network, Simon-Broome Registry]. It should be noted that LDL cholesterol cut points usually vary with age (Table 1)
.
Cardiovascular Risk Assessment: The presence of multiple cardiovascular risk factors amplifies potential risk of atherosclerosis including smoking, impaired fasting glucose/diabetes, hypertension, chronic kidney disease, presence of elevated Lipoprotein (a), metabolic syndrome, Kawasaki disease with coronary aneurysms, and possibly other chronic inflammatory conditions such as lupus are at risk for coronary artery disease as young adults.4 Results from autopsy studies of children and young adults (2 to 39 years of age), including the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study5,6 and the Bogalusa Heart Study.7,8 show that the process of atherosclerosis begins in childhood with the development of the fatty streak.5-9
Treatment: Lifestyle changes of diet and physical activity are always the first step in treating any patient with hypercholesterolemia; however, these steps are not likely to achieve the target LDL cholesterol goals in patients with HeFH. According to the AAP Guidelines1, treatment is advisable in children 10 and older with no other CHD risk when the LDL cholesterol is consistently over 190. If other risks are present, then treatment should be considered for LDL cholesterol at 160. With the presence of diabetes, LDL cholesterol of 130 should be considered for lipid lowering therapy. The target goal for patients with FH is at least 50% reduction of LDL cholesterol or LDL cholesterol 130.
Like adults, statin is the preferred initial pharmacologic treatment in children after lifestyle intervention. A number of statins have been studied for use in children ages 8 and older demonstrating good efficacy in lowering LDL cholesterol, with reasonable safety for normal pubertal development. Despite the absence of data in children demonstrating morbidity and mortality reduction by aggressive treatment of lipid disorders, the overwhelming data in adults (e.g., decreasing LDL cholesterol, improved morbidity and mortality) and evidence of atherosclerotic lesions developing in childhood support the argument for early treatment. In addition to statin therapy, colesevelam is also approved for use children to lower LDL-cholesterol, but clinical data is lacking for use of niacin, fibrates, or ezetimibe in the pediatric population.
Clinical studies which examine vascular structure and function in children with statin therapy have shown improvement in endothelial function. Recent clinical trials demonstrate early initiation of statin therapy in children with FH can delay the progression of carotid IMT in adolescents and young adults, and may also be beneficial in the prevention of atherosclerosis in adolescence.10
Homozygous FH: Children with homozygous FH have profoundly elevated LDL cholesterol levels (> 500 mg/dL) with early onset of premature CHD. It is recommended to start lipidlowering treatment younger than age 8 in homozygous FH children to reduce their marked morbidity. Even with higher doses of the more potent statins, most will require treatment with LDL apheresis in an attempt to reduce LDL cholesterol to target goals. Liver transplantation and gene therapy are potential new treatment in development. Referral to a pediatric lipid specialist is highly recommended.1,2,3
Author's Note: Special thanks are extended to Patrick McBride, MD, MPH, FACC (Faculty, University of Wisconsin School of Medicine and Public Health) for his assistance and thoughtful review of this article.
Disclosure statement: Dr. Carimi has served on the speakers' bureaus for Abbott Laboratories and Takeda Pharmaceuticals.
References for this article are listed on Page 31 of Lipid Spin PDF available here.





.jpg)
.png)











