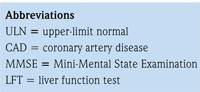
 Statin drugs have been studied in numerous controlled trials involving hundreds of thousands of study participants. Their use has resulted in reduced coronary artery disease (CAD) mortality, morbidity and, in several studies, all-cause mortality. Even though clinical trial evidence and clinical practice experience have demonstrated extremely low incidence of adverse effects, safety concerns have existed, mostly on the basis of case reports and data from clinical trials. The U.S. Food and Drug Administration (FDA) provided updates on statin labels regarding side effects in 2011 and 2012.
Statin drugs have been studied in numerous controlled trials involving hundreds of thousands of study participants. Their use has resulted in reduced coronary artery disease (CAD) mortality, morbidity and, in several studies, all-cause mortality. Even though clinical trial evidence and clinical practice experience have demonstrated extremely low incidence of adverse effects, safety concerns have existed, mostly on the basis of case reports and data from clinical trials. The U.S. Food and Drug Administration (FDA) provided updates on statin labels regarding side effects in 2011 and 2012.
Clinical trial assessment of muscle adversities
No conclusive comparative evidence exists to indicate that currently available statins differ in regard to their risks of myopathy, defined as otherwise unexplained marked creatine kinase (CK) elevation >x10 the upper-limit normal (ULN) associated with myalgia or rhabdomyolysis. The incidence of myopathy was (0.1%) for lovastatin 40mg/day and (0.2%) for lovastatin 80mg/day in the Evaluation of Xience Prime™ versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization (EXCEL) trial.1 There were no cases of myopathy or rhabdomyolysis in three major pravastatin trials.2 None of the three cases of rhabdomyolysisin patients on 10mg/day dose or the two cases on 80mg/day dose of atorvastatin in the Treating to New Targets (TNT) trial was felt by investigators to be casually related to atorvastatin.3 In an analysis of 27 Phase 2/3 controlled clinical trials of rosuvastatin, CK elevation>10X ULN occurred in 0.02% to 0.04% in a dose-independent manner. No cases of rhabdomyolysis was reported.4
The incidence of CK elevations is reported as 0.03% on 40mg/day fluvastatin and 0.00% on fluvastatin 80mg/day and there have been no reported cases of rhabdomyolysis. Therefore, fluvastatin may have the least propensity to cause myotoxicity.6 On the other hand, 10 patients – nine of them on simvastatin 80mg/day – developed myopathy in the high-risk-CAD A to Z trial.7 The highest incidence of statin-related myopathy was encountered in the seven-year, randomized, double-blind SEARCH study. Fifty-two patients (0.9%) in the 80mg group versus one patient (0.02%) in the 20mg group developed myopathy, defined as unexplained muscle weakness or pain with a serum CK >10 times ULN.8 This was higher than the labeled risk (based on clinical trial data) of 0.53%. Twenty-two patients (0.4%) in the 80mg group versus no patient in the 20mg group developed rhabdomyolysis. The risks for myopathy and rhabdomyolysis with simvastatin 80mg were highest in the first 12 months of treatment; older age and female gender both increased the risk of myopathy. In SEARCH, the risk of myopathy was approximately doubled in patients taking a calcium channel blocker, in particular diltiazem.8
The findings from the SEARCH trial are supported by analyses of the FDA's Adverse Event Reporting System (AERS) database, which show that the level of reporting of fatal rhabdomyolysis associated with the 80mg dose of simvastatin has been higher in comparison with lower doses of simvastatin or most other statins, leading to a recommendation to limit the initiation of an 80mg/day dose.
Drug interactions and metabolic pathways are major considerations. Because they are not metabolized significantly via the cytochrome P450 (CYP) pathway, pravastatin and rosuvastatin may be administered in a safer fashion if given concomitantly with drugs known to be CYP inhibitors.
Potential liver adversities
Overall, statin trials have demonstrated that the incidence of significant elevations4 1 in liver injury tests (defined as > 3 X ULN) is between 0.5% and 5%; and liver enzyme elevations are dose dependent. There is little relationship between the magnitude of low-density lipoprotein (LDL) reduction and the degree of enzyme elevation at lower doses; in other words, there are no differences between more potent statins and less potent ones. Instead, when a statin dose is doubled from the second highest to maximum allowed dose, blood transaminase levels increase. In one comparative head-to-head, six-week study involving 2,431 participants, there were only five cases of two consecutive-visit aspartate transaminase (AST) elevations on atorvastatin 80mg (n=1), atorvastatin 20mg (n=2), simvastatin 40mg (n=1), simvastatin 80mg (n=1), and none on rosuvastatin 40mg daily dose.9 The clinical significance of these often transient, self-limited elevations is unclear. The baseline measurements of liver function tests are useful for future comparisons. Pretreatment liver enzyme levels have not been predictive of clinically meaningful acute hepatocellular reactions. Therefore, routine continued monitoring of liver enzymes at lower doses of statins is not necessary except for patients on concomitant medications, with co-morbid conditions or otherwise felt to be at high risk. On Feb. 28, 2012, the FDA approved crucial changes to the safety label for statins, removing the recommendation for periodic monitoring of liver enzymes. According to the new labels, the FDA recommends that such tests be conducted before starting therapy and as clinically indicated thereafter.
Adverse renal experiences
Preclinical animal studies have demonstrated renal tubular toxicities related to high-dose statin intake. Mild proteinuria seen clinically is the result of impairment of renal tubular protein absorption by receptor-mediated endocytosis and is physiological because of HMG-CoA reductase inhibition. Hematuria seen with statin use in clinical trials commonly has other explanations. To address the question of whether urinary abnormalities with statin use are detrimental to long-term renal function, an open-label atorvastatin study was conducted. It was concluded that atorvastatin reduced the proteinuria and progression of chronic kidney disease (CKD) additive to angiotensin-convertingenzyme (ACE) Is or angiotensin-receptor blockers (ARBs). This particular beneficial or safety profile of atorvastatin may be contributed by minimal renal excretion, <2% as opposed to 10% with rosuvastatin, 13% with simvastatin and 20% with pravastatin. In the atorvastatin-based Die Deutsche Diabetes Dialyse (4D) study, no case of rhabdomyolysis was reported in 619 hemodialysis patients.11
Potential neurological adverse experiences
The level of evidence supporting potential neurological adverse effects of statins is listed in Table 1.
Case reports and clinical trials have suggested that statins may impair cognitive function, which may be of safety concern, particularly in older individuals.
.png)
In a double-blind study of 209 generally healthy hypercholesterolemic adults, randomly assigned to six-month treatment with lovastatin 20 mg or a placebo, lovastatin did not cause psychological distress or substantially alter cognitive function, but it did result in small performance decrements on neuropsychological tests of attention and psychomotor speed, which were concluded to be of uncertain clinical importance. In a similar follow-up study of 308 adults with hypercholesterolemia, a randomized, double-blind, placebocontrolled trial of simvastatin 10mg or 40mg for six months provided partial support for minor decrements in cognitive functioning with statins. In the Pravastatin in Elderly Individuals at Risk of Vascular Disease (PROSPER) trial, the largest statin trial conducted specifically in older study participants, 5,804 men and women ages 70 to 82 years with a history of or risk factors for vascular disease were evaluated for mental changes. After an average of 3.2 years, pravastatin 40mg/day was found to have no significant effect on cognitive function or disability compared with a placebo, as assessed by diagnostic instruments such as the Mini-Mental State Examination (MMSE). With specific regard to dementia (which may include Alzheimer’s disease), nested case-control designed studies revealed that individuals who were prescribed statins actually had a substantially lowered risk of developing dementia. However, a meta-analysis based on the Cochrane database review (pooling the studies providing a change in MMSE from baseline) of the effect of statins on dementia concluded that, while there was insufficient evidence to recommend statins for the treatment of dementia, statins were not detrimental to cognitive function.
An FDA review concluded that data from the observational studies and clinical trials did not suggest that cognitive changes associated with statin use were common or led to clinically significant cognitive decline, but information about the potential for generally non-serious and reversible cognitive side effects (memory loss, confusion, etc.) was added to the statin labels.
Peripheral nervous system
In case reports, and in a small number of case-control and cohort studies it is suggested that statins may be associated with peripheral nervous system adverse experiences. However, from a review of the literature, it is reasonable to conclude that any potential risk of peripheral neuropathy with statin use is very small. A stepwise approach to the patient with a potential statin-related peripheral neuropathy adverse experience may be to, first, ensure that other secondary causes have been evaluated; second, to perform a neurologic physical examination and attempt to objectively quantify abnormal neurologic physical findings; and third, to obtain appropriate diagnostic neurologic studies; and, fourth, to stop administering the statin. If objective abnormalities are found on physical examination and diagnostic neurologic testing, and if the neuropathic symptoms resolve upon discontinuing the statin, then it may be useful to repeat the objective evaluations to see whether the resolution of symptoms correlates with the resolution of objective neurologic findings. If resolution of symptoms or objective neurologic testing does not occur after withdrawal of statin therapy, then the diagnosis of idiopathic peripheral neuropathy unrelated to statin use should be considered. Conversely, if symptoms and objective neurologic testing resolve, then the clinician can best decide whether the benefits of a re-challenge of a statin drug exceeds the potential risks.
Increases in glycosylated hemoglobin (HbA1c) and fasting plasma glucose
In the FDA’s review of the results from the Justification for the Use of Statins in Primary Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) trial, it was reported that there was a 27% increase in investigator-reported diabetes mellitus in rosuvastatin-treated patients compared to placebo-treated patients. High-dose atorvastatin also has been associated with worsening glycemic control in the Pravastatin or Atorvastatin Evaluation and Infection Therapy – Thrombolysis in Myocardial Infarction 22 Investigators (PROVE-IT TIMI 22) substudy. A metaanalysis by Sattar, et al., reported that statin therapy was associated with a 9% increased risk for incident diabetes (odds ratio [OR] 1.09[1.02-1.17]), with little heterogeneity (I2=11%) between trials.19 A meta-analysis by Rajpathak also reported a small increase in diabetes risk (relative risk [RR] 1.13[1.03-1.23]) with no evidence of heterogeneity across trials.21 A recent study by Culver, et al., using data from the Women’s Health Initiative, reported that statin use conveys an increased risk of new-onset diabetes in postmenopausal women and noted that the effect appears to be a medication-class effect, unrelated to potency or to individual statin type22 contrary to the findings of Carter.23 In this 14-year observational study, a relationship between the potency (and duration) of statin therapy and the incidence of diabetes development was observed. However, the selection bias of a higher-risk population requiring more intense statin therapy could not be excluded.23 Based on clinical trial meta-analyses and epidemiological data from the published literature, information concerning an effect of statins on incident diabetes and increases in HbA1c and/or fasting plasma glucose was added to statin labels.
Disclosure statement: Dr. Baykal has received consulting fees from Actelion Pharmaceuticals Ltd.





.jpg)
.png)











